INTRODUCTION:
Type 2 diabetes, once considered a disease predominantly affecting adults, has been rapidly increasing among children in recent years. This alarming trend has raised significant concerns among healthcare professionals and parents alike. Type 2 diabetes, characterized by insulin resistance and high blood sugar levels, poses serious health risks for children, including long-term complications. This article explores the causes, risk factors, consequences, and potential preventive measures associated with the rise of type 2 diabetes in children.
RISING PREVALENCE:
Several factors contribute to the rising prevalence of type 2 diabetes in children:
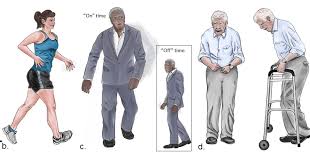
- Childhood Obesity Epidemic: One of the primary drivers of pediatric type 2 diabetes is the epidemic of childhood obesity. The increasing prevalence of unhealthy eating habits, sedentary lifestyles, and reduced physical activity has led to a significant rise in overweight and obese children. Excess weight and obesity are closely linked to insulin resistance, a key factor in the development of type 2 diabetes.
- Sedentary Lifestyles: Modern society’s shift towards sedentary activities, such as excessive screen time and reduced physical exercise, has contributed to the increased incidence of type 2 diabetes in children. Insufficient physical activity not only promotes weight gain but also exacerbates insulin resistance.
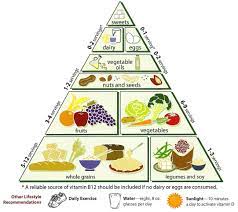
- Unhealthy Dietary Patterns: Poor dietary choices, including a high consumption of sugary beverages, processed foods, and fast food, coupled with a low intake of nutrient-dense foods like fruits, vegetables, and whole grains, significantly contribute to the development of type 2 diabetes in children. Such diets often lead to excessive calorie intake, weight gain, and insulin dysregulation.
- Genetic Predisposition: While lifestyle factors play a crucial role in the development of type 2 diabetes, genetic predisposition can also contribute to a child’s susceptibility to the disease. Children with a family history of type 2 diabetes are at higher risk of developing the condition themselves.
IMPLICATIONS:
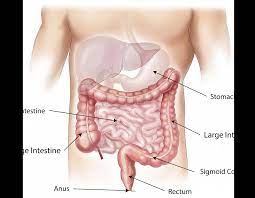
The implications of the rising prevalence of type 2 diabetes in children are far-reaching. This chronic condition can lead to severe health complications and impact a child’s overall well-being. Uncontrolled type 2 diabetes in childhood may increase the risk of cardiovascular disease, kidney damage, nerve damage, vision problems, and other related health issues. Additionally, children diagnosed with diabetes face lifelong management of their condition, including the need for regular blood sugar monitoring, medication, and lifestyle modifications.
ADRESSING THE ISSUE:
To combat the increasing prevalence of type 2 diabetes in children, a comprehensive approach is required:
- Prevention through Education: Educating children, parents, and communities about the importance of healthy eating habits, regular physical activity, and weight management is essential. Emphasizing the long-term consequences of type 2 diabetes and empowering individuals to make informed choices can help prevent its onset.
- Healthier Environments: Schools and communities should provide opportunities for physical activity, promote nutritious meals, and discourage the consumption of sugary beverages and unhealthy snacks. Creating supportive environments that encourage healthy habits can contribute to reducing the prevalence of type 2 diabetes.
- Early Screening and Diagnosis: Regular health check-ups should include screenings for type 2 diabetes risk factors, especially among children with a family history of the disease or those who are overweight or obese. Early detection allows for timely intervention and management.
- Collaborative Efforts: Healthcare providers, policymakers, schools, and parents must work together to address the rising prevalence of type 2 diabetes in children. Policies that support healthy school environments, community programs promoting physical activity, and increased access to nutritious foods are vital in curbing this trend.
CAUSES AND RISK FACTORS:
- Obesity and Excess Weight: Obesity is a significant risk factor for type 2 diabetes. Excess body fat, particularly around the abdomen (central obesity), is strongly linked to insulin resistance. Adipose tissue releases substances that interfere with insulin action, leading to elevated blood sugar levels.
- Sedentary Lifestyle: Lack of regular physical activity and a sedentary lifestyle contribute to the development of type 2 diabetes. Physical activity plays a crucial role in maintaining healthy body weight, improving insulin sensitivity, and promoting glucose metabolism.
- Unhealthy Diet: Consuming a diet high in refined carbohydrates, saturated and trans fats, sugary beverages, and processed foods contributes to the development of type 2 diabetes. These dietary choices lead to weight gain, insulin resistance, and impaired glucose regulation.
- Family History and Genetics: Family history and genetic factors play a role in the development of type 2 diabetes. Having a parent or sibling with the condition increases the risk. Certain genes associated with insulin production, insulin action, and metabolism can contribute to an individual’s susceptibility to type 2 diabetes.
- Age: Advancing age is a significant risk factor for type 2 diabetes. While the condition can occur at any age, the risk increases with age, particularly after the age of 45. This is partly due to age-related weight gain, decreased physical activity, and decreased pancreatic function.
- Ethnicity: Certain ethnic groups, such as African Americans, Hispanic/Latino Americans, Native Americans, Asian Americans, and Pacific Islanders, have a higher predisposition to type 2 diabetes compared to the general population. Genetic and lifestyle factors specific to these populations contribute to the increased risk.
- Gestational Diabetes: Women who have had gestational diabetes (diabetes during pregnancy) are at an increased risk of developing type 2 diabetes later in life. Additionally, their children may also have a higher risk of developing the condition.
- Polycystic Ovary Syndrome (PCOS): PCOS is a hormonal disorder that affects women and is characterized by irregular menstrual cycles, excess androgen levels, and insulin resistance. Women with PCOS have an increased risk of developing type 2 diabetes.
- Hypertension (High Blood Pressure): Hypertension is often associated with type 2 diabetes, and the two conditions commonly coexist. The mechanisms underlying their relationship are complex, but both conditions share common risk factors, such as obesity and unhealthy lifestyles.
- Other Medical Conditions: Certain medical conditions, such as metabolic syndrome, impaired glucose tolerance, and acanthosis nigricans (a skin condition characterized by darkened patches), are associated with an increased risk of type 2 diabetes.
DIFFERENT DIAGNOSING FACTORS:
It’s important to note that while these factors contribute to the development of type 2 diabetes, not everyone with these risk factors will develop the condition. Additionally, there may be other contributing factors not listed here, as the disease’s causes are still being researched.
- Fasting Plasma Glucose (FPG) Test: This blood test measures the blood sugar level after fasting for at least 8 hours. A fasting plasma glucose level of 126 mg/dL (7.0 mmol/L) or higher on two separate occasions generally indicates diabetes.
- Oral Glucose Tolerance Test (OGTT): This test measures the blood sugar level after fasting and then consuming a glucose-rich drink. Blood sugar levels are checked at regular intervals over a few hours. A blood sugar level of 200 mg/dL (11.1 mmol/L) or higher after 2 hours during the OGTT is indicative of diabetes.
- Hemoglobin A1c (HbA1c) Test: The HbA1c test provides an estimate of average blood sugar levels over the past 2 to 3 months. A result of 6.5% or higher is typically considered indicative of diabetes.
- Random Plasma Glucose Test: In some cases, a random plasma glucose test may be performed. It measures blood sugar levels regardless of when the individual last ate. A result of 200 mg/dL (11.1 mmol/L) or higher, along with typical symptoms of diabetes, may indicate diabetes.
- Glycated Albumin (GA) Test: The GA test measures the amount of glycated albumin, a protein that reflects short-term blood sugar control, over a 2 to 3 week period. It can be useful in situations where the HbA1c test may not be reliable, such as in individuals with certain medical conditions.
- Other Laboratory Tests: Additional laboratory tests may be conducted to assess overall health and potential complications associated with diabetes. These may include tests for kidney function, lipid profile (cholesterol levels), liver function, and urine tests to check for protein or ketones.
It’s important to note that the specific diagnostic criteria and tests may vary between different countries and healthcare guidelines. Additionally, a healthcare professional will consider the individual’s clinical presentation, risk factors, and other relevant factors when making a diagnosis.
MANAGEMENT:
Management of Type 2 Diabetes Mellitus:
If you have been diagnosed with type 2 diabetes, it’s important to actively manage the condition to maintain optimal blood sugar control and reduce the risk of complications. Here are key strategies for managing type 2 diabetes:
- Healthy Eating:
- Follow a balanced diet: Eat a variety of nutritious foods, including fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit the intake of processed foods, sugary snacks, and beverages.
- Portion control: Be mindful of portion sizes to manage carbohydrate intake and help regulate blood sugar levels.
- Regular meal schedule: Establish regular meal times and spacing to support consistent blood sugar control.
- Regular Physical Activity:
- Engage in aerobic exercises: Include activities like brisk walking, cycling, swimming, or dancing in your routine. Aim for at least 150 minutes of moderate-intensity aerobic activity per week.
- Strength training: Incorporate resistance exercises to build muscle strength, which can improve insulin sensitivity and blood sugar control.
- Stay active throughout the day: Avoid long periods of sitting or inactivity. Take short breaks to move or stretch, especially after meals.
- Medication Management:
- Follow prescribed medications: Take medications as directed by your healthcare provider to control blood sugar levels. This may include oral medications or insulin injections.
- Regularly monitor blood sugar levels: Check your blood glucose levels as recommended by your healthcare provider. This helps track your progress and adjust medications as needed.
- Understand medication side effects: Be aware of potential side effects and discuss any concerns or changes with your healthcare provider.
- Blood Sugar Monitoring:
- Monitor blood sugar levels: Regularly check and record your blood glucose levels using a glucometer or continuous glucose monitoring system, as advised by your healthcare provider.
- Track patterns and make adjustments: Monitor trends in your blood sugar readings to identify patterns. Adjust your diet, exercise, and medication regimen accordingly, with guidance from your healthcare provider.
- Regular Medical Check-ups:
- Schedule regular check-ups: Visit your healthcare provider at recommended intervals for comprehensive diabetes care, including monitoring of blood pressure, cholesterol levels, kidney function, and other relevant tests.
- Eye and foot examinations: Regularly undergo eye exams to detect and manage any diabetes-related eye complications. Additionally, have regular foot exams to identify any potential foot problems associated with diabetes.
- Diabetes Self-Management Education:
- Seek diabetes education and support: Attend diabetes education programs to enhance your knowledge of self-care techniques, meal planning, medication management, and coping strategies.
- Collaborate with healthcare professionals: Work closely with your healthcare team, including doctors, diabetes
- educators, nutritionists, and pharmacists, to develop an individualized management plan.
- Stress Management and Emotional Well-being:
- Practice stress-reducing techniques: Engage in activities like meditation, deep breathing exercises, yoga, or hobbies that promote relaxation and reduce stress levels.
- Seek emotional support: Connect with support groups, friends, or family members who can provide understanding and encouragement. Consider seeking professional counseling if needed.
- Lifestyle Modifications:
- Quit smoking: If you smoke, seek help to quit smoking, as smoking worsens diabetes complications.
- Limit alcohol intake: Moderate alcohol consumption is generally recommended. Discuss with your healthcare provider about alcohol guidelines that are appropriate for you.
- Remember, individual management plans may vary based on personal circumstances, and it’s important to work closely with your healthcare team to develop a plan that suits your specific needs. With proper management and self-care, individuals with type 2 diabetes can lead healthy, fulfilling lives while effectively managing their condition.


I’m definitely bookmarking this for future reference.
Your tips are always so practical.
I found this post incredibly helpful. The step-by-step approach you’ve taken is very useful, and I’ve learned a lot that I can apply to my own projects.
Thank you for this informative and engaging article. The examples you’ve provided make it much easier to understand the concepts you’re discussing.