INTRODUCTION:
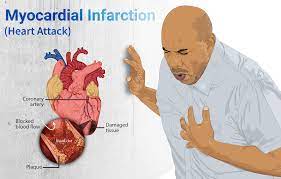
Myocardial infarction, commonly known as a heart attack, is a serious medical condition that occurs when there is a prolonged interruption of blood supply to a part of the heart muscle. This interruption is usually caused by the complete blockage of a coronary artery, which is responsible for supplying oxygen-rich blood to the heart.
The most common cause of a myocardial infarction is the rupture of a plaque within a coronary artery, leading to the formation of a blood clot that obstructs blood flow. This can occur due to the buildup of fatty deposits (atherosclerosis) within the artery walls over time.
During a heart attack, the affected part of the heart muscle doesn’t receive enough oxygen, and if blood flow is not restored promptly, the muscle tissue can be permanently damaged or even die. The severity of a heart attack can vary, depending on the extent of the blockage and the size of the affected area.
SYMPTOMS OF MI:
The symptoms of a myocardial infarction (heart attack) can vary from person to person. While some individuals may experience classic symptoms, others may have atypical or milder symptoms. It’s important to note that not everyone will have the same set of symptoms, and some people may even have a silent heart attack with no noticeable symptoms. However, here are the common symptoms associated with a heart attack:
- Chest pain or discomfort: This is the most common symptom of a heart attack. The pain or discomfort is typically located in the center or left side of the chest and can be described as a tightness, pressure, squeezing, or crushing sensation. It may last for a few minutes or longer. Some individuals may mistake it for indigestion or heartburn.
- Pain or discomfort in other upper body areas: The pain can radiate from the chest to other areas such as the left arm, both arms, jaw, neck, back, or even the stomach. The intensity of pain in these areas can vary.
- Shortness of breath: Feeling breathless or having difficulty breathing, even with minimal physical exertion or at rest, can be a symptom of a heart attack.
- Sweating: Profuse sweating that is not related to exercise or external factors may occur during a heart attack. The skin may feel clammy or cold.
- Nausea, vomiting, or indigestion: Some individuals may experience feelings of nausea, and occasionally vomiting, as a symptom of a heart attack. They may also experience indigestion-like symptoms, including abdominal discomfort or a feeling of fullness.
- Lightheadedness or dizziness: Feeling lightheaded or dizzy, sometimes accompanied by fainting or near-fainting, can occur during a heart attack.
- Fatigue or extreme weakness: Unusual or extreme tiredness, without any apparent reason, may be a symptom of a heart attack.
It’s important to note that these symptoms can vary in their presentation and intensity. Some individuals may experience only mild symptoms, while others may have more severe symptoms. Additionally, some people, particularly women, older adults, and those with diabetes, may have atypical symptoms or milder presentations, which can include unexplained fatigue, shortness of breath, or discomfort in the neck, jaw, or upper back.
If you or someone else experiences symptoms that could indicate a heart attack, it is crucial to seek immediate medical attention by calling emergency services. Prompt medical care can significantly improve the outcome and minimize heart damage.
PREVENTIVE MEASURES:
Preventive measures for reducing the risk of myocardial infarction (MI) or heart attack involve adopting a heart-healthy lifestyle and managing risk factors. Here are some preventive measures you can take:
- Quit smoking: Smoking is a major risk factor for heart disease, including MI. Quitting smoking significantly reduces the risk of heart attacks. Seek support from healthcare professionals or join smoking cessation programs to help you quit successfully.
- Adopt a healthy diet: Follow a balanced diet that is low in saturated and trans fats, cholesterol, and sodium (salt). Instead, focus on consuming fruits, vegetables, whole grains, lean proteins (such as fish and poultry), and healthy fats (such as those found in nuts, seeds, and olive oil).
- Maintain a healthy weight: Aim to maintain a body weight within a healthy range. Losing excess weight, especially around the waistline, can reduce the risk of heart disease. Consult with a healthcare professional to determine a suitable weight loss plan if needed.
- Engage in regular physical activity: Aim for at least 150 minutes of moderate-intensity aerobic exercise or 75 minutes of vigorous-intensity exercise each week. Regular physical activity helps maintain a healthy weight, lowers blood pressure, improves cholesterol levels, and reduces the risk of heart disease.
- Manage hypertension (high blood pressure): If you have high blood pressure, work with your healthcare provider to develop a plan to manage it effectively. This may involve lifestyle modifications, such as reducing sodium intake, regular exercise, and medications if necessary.
- Control cholesterol levels: High levels of LDL (bad) cholesterol and low levels of HDL (good) cholesterol increase the risk of heart disease. Follow a heart-healthy diet, exercise regularly, and consider medications prescribed by your healthcare provider if lifestyle changes alone are not enough to manage cholesterol levels.
- Manage diabetes: Keep blood sugar levels under control if you have diabetes. Monitor your blood sugar regularly, follow your healthcare provider’s advice regarding medication, diet, and lifestyle modifications.
- Manage stress: Chronic stress can contribute to the risk of heart disease. Find healthy ways to manage stress, such as regular exercise, relaxation techniques (such as deep breathing or meditation), hobbies, and social support.
- Limit alcohol consumption: Excessive alcohol consumption can raise blood pressure and increase the risk of heart disease. If you choose to drink, do so in moderation, which is up to one drink per day for women and up to two drinks per day for men.
- Regular medical check-ups: Schedule regular check-ups with your healthcare provider to monitor your overall health, manage risk factors, and detect any underlying conditions or concerns early.
Remember, it’s important to consult with your healthcare provider for personalized advice and guidance on preventive measures based on your individual risk factors and medical history. They can provide you with appropriate recommendations tailored to your specific needs.
DIFFERENT DIAGNOSING FACTORS:
To evaluate the stages of myocardial infarction (MI) or a heart attack, various tests and procedures may be performed. These tests help in diagnosing and assessing the extent of damage to the heart. Here are some common tests used to evaluate the stages of MI:
- Electrocardiogram (ECG): An ECG is a non-invasive test that records the electrical activity of the heart. It can help diagnose a heart attack and determine its location and severity. Changes in the ECG pattern, such as ST-segment elevation or depression, can indicate myocardial damage.
- Blood tests: Blood tests are done to measure certain markers that indicate heart muscle damage. The most commonly measured markers are cardiac troponins (troponin T and troponin I). Elevated levels of these markers in the blood suggest a heart attack
- A)Cardiac Troponin: Troponin is a cardiac-specific protein released into the bloodstream when heart muscle cells are damaged. Troponin levels rise within a few hours of a heart attack and remain elevated for a period of time. Blood tests measure troponin levels to confirm the diagnosis of MI and assess the extent of cardiac damage. There are two types of troponin: Troponin T (cTnT) and Troponin I (cTnI). Elevated levels of either or both indicate myocardial damage.
- Creatine Kinase (CK) and CK-MB: Creatine Kinase is an enzyme found in various tissues, including the heart muscle. In the blood, CK is further divided into different subtypes, including CK-MB, which is more specific to heart muscle cells. Elevated levels of CK-MB can indicate myocardial damage.
- Myoglobin: Myoglobin is a protein found in heart and skeletal muscles. It is released into the bloodstream following muscle injury, including heart muscle damage. Elevated levels of myoglobin can indicate a heart attack. However, myoglobin is not as specific to the heart as troponin, so it is often used in conjunction with other cardiac markers.
- Echocardiogram: An echocardiogram uses ultrasound waves to create images of the heart’s structure and function. It helps evaluate the pumping function of the heart, assess the size and location of the infarction, and identify any complications such as heart valve problems or reduced blood flow.
- Coronary angiography: Coronary angiography is an invasive procedure that involves injecting a contrast dye into the coronary arteries. X-ray images are then taken to visualize the blood flow and detect any blockages or narrowing in the arteries. This procedure helps determine the location and severity of coronary artery disease, which may have caused the heart attack.
- Cardiac MRI: A cardiac magnetic resonance imaging (MRI) provides detailed images of the heart, allowing assessment of the heart’s structure, function, and blood flow. It can help identify the size and location of the heart attack, as well as assess any damage to the heart muscle.
- Exercise stress test: An exercise stress test measures how the heart responds to physical activity. During the test, you will be asked to walk on a treadmill or ride a stationary bike while your heart’s activity is monitored. This test helps evaluate how well the heart is functioning after a heart attack and assesses exercise tolerance.
- Nuclear imaging: Nuclear imaging involves injecting a radioactive tracer into the bloodstream, which is taken up by the heart muscle. Scans are then performed to detect areas of reduced blood flow or damaged heart tissue.
These are some of the common tests used to evaluate the stages of a myocardial infarction. The specific tests recommended may vary depending on the individual’s condition and the clinical judgment of the healthcare provider. It’s important to consult with a healthcare professional for an accurate diagnosis and appropriate testing based on your specific situation.
DIET TO BE FOLLOWED:
Following a heart-healthy diet is crucial for individuals who have experienced a myocardial infarction (MI) or want to reduce the risk of heart disease. Here are some foods that are generally recommended for individuals with MI:
- Fruits and vegetables: Incorporate a variety of fruits and vegetables into your diet. They are rich in vitamins, minerals, antioxidants, and fiber, which can help reduce the risk of heart disease. Aim for at least five servings of fruits and vegetables each day.
- Whole grains: Choose whole grains over refined grains. Whole grains like whole wheat, oats, brown rice, quinoa, and barley provide fiber, which helps lower cholesterol levels and maintain heart health.
- Lean proteins: Opt for lean sources of protein such as skinless poultry, fish (such as salmon, trout, and tuna), legumes (beans, lentils, and peas), and tofu. Limit red meat consumption and choose lean cuts when consumed.
- Healthy fats: Include healthy fats in your diet, such as those found in avocados, nuts (like almonds, walnuts, and pistachios), seeds (such as chia seeds and flaxseeds), and olive oil. These fats are monounsaturated and polyunsaturated fats that can help improve heart health.
- Fatty fish: Fatty fish like salmon, mackerel, sardines, and trout are rich in omega-3 fatty acids. Omega-3 fatty acids have been shown to have beneficial effects on heart health, including reducing the risk of heart disease and improving overall cardiovascular health. Aim to include fatty fish in your diet at least twice a week.
- Low-fat dairy products: Choose low-fat or skim milk, yogurt, and cheese to reduce saturated fat intake. Calcium and vitamin D from dairy products can still be beneficial for heart health.
- Legumes and beans: Legumes and beans, such as lentils, chickpeas, kidney beans, and black beans, are excellent sources of fiber and plant-based protein. They are low in fat and can be a healthy alternative to meat.
- Nuts and seeds: Enjoy a moderate amount of nuts and seeds as a snack or added to meals. They provide heart-healthy fats, fiber, and other beneficial nutrients. However, be mindful of portion sizes as they are high in calories.
- Limited sodium: Reduce your intake of sodium by avoiding processed and packaged foods, which are often high in sodium. Instead, flavor your food with herbs, spices, and natural seasonings.
- Water: Stay hydrated by drinking an adequate amount of water throughout the day. It is important for overall health and helps maintain proper heart function.
Remember that maintaining a heart-healthy diet should be part of an overall healthy lifestyle. It is recommended to consult with a registered dietitian or healthcare professional to develop a personalized diet plan that suits your specific dietary needs, preferences, and medical condition. They can provide you with specific guidance and recommendations based on your individual situation.
TREATMENT:
The treatment for myocardial infarction (MI), or a heart attack, aims to restore blood flow to the blocked coronary artery, minimize damage to the heart muscle, prevent complications, and reduce the risk of future heart events. The specific treatment options may vary depending on the individual’s condition and the severity of the heart attack. Here are some common treatment approaches:
- Medications:
- Thrombolytics or clot-busting drugs: These medications are administered as soon as possible after a heart attack to dissolve the blood clot causing the blockage in the coronary artery.
- Antiplatelet drugs: Medications like aspirin, clopidogrel, or ticagrelor are prescribed to prevent the formation of new blood clots and reduce the risk of further blockages.
- Beta-blockers: These drugs help reduce the workload on the heart, decrease blood pressure, and slow the heart rate, thereby protecting the heart muscle and preventing arrhythmias.
- ACE inhibitors or angiotensin receptor blockers (ARBs): These medications are often prescribed to improve heart function, lower blood pressure, and reduce the risk of future cardiovascular events.
- Statins: These drugs are prescribed to lower cholesterol levels and reduce the risk of plaque buildup in the arteries.
- Other medications: Depending on the individual’s condition, additional medications may be prescribed to manage symptoms, control blood pressure, or address specific cardiac concerns.
- Reperfusion Therapy:
- Percutaneous Coronary Intervention (PCI): Also known as angioplasty, this procedure involves inserting a catheter with a balloon at the tip into the blocked coronary artery. The balloon is then inflated to open the narrowed or blocked artery, and a stent (a tiny mesh tube) may be placed to keep the artery open and restore blood flow.
- Coronary Artery Bypass Grafting (CABG): In cases where PCI is not feasible or appropriate, CABG surgery may be recommended. This procedure involves creating new routes for blood flow by using a graft to bypass the blocked coronary artery.
- Cardiac Rehabilitation:
- Cardiac rehabilitation is a comprehensive program that includes supervised exercise, education, counseling, and support to help individuals recover from a heart attack and improve their overall heart health.
- Lifestyle Modifications:
- Adopting a heart-healthy diet, low in saturated and trans fats, cholesterol, and sodium, and rich in fruits, vegetables, whole grains, lean proteins, and healthy fats.
- Engaging in regular physical activity as recommended by healthcare professionals.
- Quitting smoking and avoiding exposure to secondhand smoke.
- Managing and controlling other risk factors like high blood pressure, high cholesterol, diabetes, and obesity.
- Managing stress through relaxation techniques, counseling, or stress management programs.
Treatment for myocardial infarction requires individualized care, and the specific treatment plan will depend on the patient’s medical history, overall health, and the severity of the heart attack. It’s important to consult with a healthcare professional for accurate diagnosis, appropriate treatment, and ongoing care.