Horner’s Syndrome is a rare neurological condition characterized by a specific combination of symptoms affecting the eye, eyelid, and facial muscles. It can result from various underlying causes, ranging from trauma and neurological disorders to congenital factors. Prompt diagnosis and identification of the underlying cause are essential for appropriate management and treatment. While there is no specific cure for Horner’s Syndrome, addressing the underlying condition, managing symptoms, and ensuring regular monitoring can significantly improve the quality of life for individuals affected by this condition.
CAUSES AND MECHANISM:
Causes and Mechanism:Horner’s Syndrome occurs when there is an interruption or disruption in the sympathetic nerve pathway that runs from the brain to the face. The disruption can arise from various underlying causes, including:
- Injury: Trauma or injury to the head, neck, or chest, such as a car accident or surgical intervention, can damage the sympathetic nerves and lead to Horner’s Syndrome.
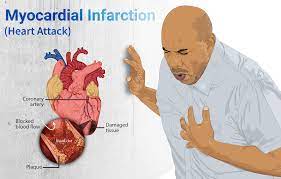
- Neurological Conditions: Certain neurological conditions like stroke, tumors, multiple sclerosis, or brainstem lesions can affect the sympathetic nerve pathway and cause Horner’s Syndrome.
- Infections: In rare cases, infections such as herpes zoster (shingles) or tuberculosis can result in Horner’s Syndrome.
- Congenital Causes: Horner’s Syndrome can be present at birth (congenital) due to abnormalities or developmental issues affecting the sympathetic nerves.
SYMPTOMS:
The characteristic signs and symptoms of Horner’s Syndrome include:
- Ptosis: Drooping of the upper eyelid on the affected side, caused by the disruption of the muscles responsible for raising the eyelid.
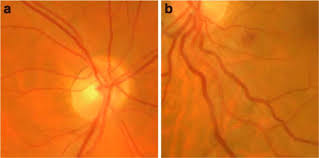
- Miosis: Constriction of the pupil on the affected side, leading to a smaller pupil compared to the other eye.
- Anhidrosis: Reduced or absent sweating on the affected side of the face, often noticed during physical exertion or exposure to heat.
- Facial Anomalies: In some cases, additional facial manifestations may be present, such as slight differences in skin color or decreased blood flow to the affected side.
DIAGNOSIS AND TREATMENT:
Diagnosing Horner’s Syndrome involves a comprehensive evaluation of the patient’s medical history, a thorough physical examination, and specialized tests. These may include:
- Pharmacological Testing: Eye drops containing specific medications, such as phenylephrine or apraclonidine, can be administered to assess the pupil response and help determine the location of the sympathetic nerve pathway disruption.
- Imaging Studies: Imaging techniques like magnetic resonance imaging (MRI) or computed tomography (CT) scans may be conducted to evaluate the structures of the brain, neck, and chest to identify potential underlying causes.
- Additional Testing: Depending on the suspected cause, further tests may be necessary to investigate underlying conditions or abnormalities, such as blood tests, nerve conduction studies, or lumbar puncture.
Treatment for Horner’s Syndrome focuses on managing the underlying cause and alleviating symptoms. As the syndrome is often secondary to an underlying condition, treatment may involve addressing the primary disorder, such as surgical intervention, medication, or other appropriate therapies. In cases where no underlying cause is identified or the symptoms are mild, no specific treatment may be necessary, and the condition may resolve on its own.
CONCLUSION:
Horner’s Syndrome is a rare neurological condition characterized by a specific combination of symptoms affecting the eye, eyelid, and facial muscles. It can result from various underlying causes, ranging from trauma and neurological disorders to congenital factors. Prompt diagnosis and identification of the underlying cause are essential for appropriate management and treatment. While there is no specific cure for Horner’s Syndrome, addressing the underlying condition, managing symptoms, and ensuring regular monitoring can significantly improve the quality of life for individuals affected by this condition.