INTRODUCTION :
Diabetic retinopathy is a serious eye condition that affects individuals with diabetes. It is one of the leading causes of blindness worldwide, and its prevalence is steadily increasing with the growing diabetes epidemic.
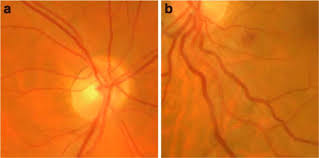
UNDERSTANDING DIABETIC RETINOPATHY:
Diabetic retinopathy is a complication of diabetes that affects the blood vessels in the retina, the light-sensitive tissue at the back of the eye. High blood sugar levels associated with diabetes can damage the blood vessels, leading to their leakage or abnormal growth. This can result in vision impairment or, in severe cases, blindness if left untreated.
CAUSES AND RISK FACTORS:
The exact cause of diabetic retinopathy is not fully understood, but several factors contribute to its development. Prolonged high blood sugar levels, high blood pressure, high cholesterol, and the duration of diabetes are significant risk factors. Additionally, individuals with poorly managed diabetes, especially those with type 1 diabetes, are more prone to developing this condition.
SYMPTOMS:
Diabetic retinopathy progresses through several stages, each characterized by specific changes in the retina. It is essential to understand these stages and recognize the associated symptoms to seek timely medical attention. Here are the stages and symptoms of diabetic retinopathy:
- Mild Non-proliferative Retinopathy:
- Symptoms: Usually no noticeable symptoms at this stage.
- Retinal Changes: Microaneurysms (small bulges in blood vessels) may appear in the retina.
- Moderate Non-proliferative Retinopathy:
- Symptoms: Mild vision problems, such as blurred or distorted vision.
- Retinal Changes: Blood vessels supplying the retina may become blocked, leading to decreased blood flow.
- Severe Non-proliferative Retinopathy:
- Symptoms: More pronounced vision problems, including difficulty seeing in low light and decreased peripheral vision.
- Retinal Changes: Many blood vessels become blocked, depriving the retina of essential nutrients and oxygen. This triggers the growth of new blood vessels, a condition called proliferative retinopathy.
- Proliferative Retinopathy:
- Symptoms: Vision problems become more severe and can include floaters, sudden vision loss, or even blindness.
- Retinal Changes: Fragile, abnormal blood vessels proliferate on the surface of the retina and optic nerve. These new blood vessels are prone to leakage, causing retinal detachment and severe vision impairment.
It is important to note that diabetic retinopathy can affect both eyes, although the progression may vary in each eye. Additionally, some individuals may not experience noticeable symptoms until the later stages of the disease. Therefore, regular eye examinations, especially for individuals with diabetes, are crucial for early detection and appropriate management of diabetic retinopathy.
If you are experiencing any changes in your vision or have diabetes, it is essential to consult an eye care professional for a comprehensive eye examination. Remember, early intervention and treatment can significantly improve the outcomes and help preserve your vision.
DIAGNOSIS:
Regular eye examinations are crucial for detecting and monitoring diabetic retinopathy. An ophthalmologist will perform a comprehensive eye exam, including a visual acuity test, dilated eye exam, and possibly imaging tests like optical coherence tomography (OCT) or fluorescein angiography to assess the extent of retinal damage.
TREATMENT OPTIONS:
The treatment for diabetic retinopathy depends on the stage and severity of the condition. In the early stages, maintaining good blood sugar control, blood pressure management, and cholesterol control are essential. Additionally, lifestyle modifications, such as a healthy diet, regular exercise, and smoking cessation, can help slow down the progression of the disease.
In more advanced stages, treatment options may include laser photocoagulation, which helps to seal leaking blood vessels, or intravitreal injections of medications called anti-vascular endothelial growth factors (anti-VEGF) to reduce abnormal blood vessel growth. In severe cases, vitrectomy, a surgical procedure to remove blood or scar tissue from the eye, may be necessary.
PREVENTION AND SELF CARE:
Prevention plays a crucial role in managing diabetic retinopathy. It is essential for individuals with diabetes to control their blood sugar levels through proper diet, regular exercise, and adherence to prescribed medications. Routine eye examinations, at least once a year, are recommended to detect any early signs of retinopathy.
CONCLUSION :
Diabetic retinopathy is a significant concern for individuals with diabetes, as it can lead to vision loss and blindness if not properly managed. Regular eye exams, early detection, and appropriate treatment can help prevent or slow down the progression of the disease. Managing diabetes effectively and adopting a healthy lifestyle are essential for reducing the risk of developing diabetic retinopathy. By raising awareness and prioritizing eye health, we can combat this silent threat and preserve vision for individuals living with diabetes.