INTRODUCTION:
Coeliac disease, also known as celiac disease, is an autoimmune disorder that affects the small intestine. It is triggered by the consumption of gluten, a protein found in wheat, barley, and rye. When individuals with coeliac disease consume gluten, their immune system reacts by damaging the lining of the small intestine, leading to various health complications.
CAUSES OF COELIAC DISEASE:
The exact cause of coeliac disease is still unknown, but it is believed to involve a combination of genetic and environmental factors. People with a family history of the disease are at a higher risk of developing it. Certain genetic markers, such as HLA-DQ2 and HLA-DQ8, are associated with an increased susceptibility to coeliac disease. Other factors, such as the timing of gluten introduction into an infant’s diet and the composition of the gut microbiome, may also play a role.
SYMPTOMS:
Symptoms of coeliac disease can vary among individuals and may affect different body systems. Some common symptoms include:
- Digestive Issues: Abdominal pain, bloating, gas, diarrhea, constipation, and vomiting are common digestive symptoms. These symptoms may occur after consuming gluten-containing foods.
- Weight Loss and Malnutrition: Unintended weight loss and malnutrition can result from the malabsorption of nutrients caused by damage to the small intestine. Deficiencies in essential vitamins, minerals, and nutrients can lead to fatigue, weakness, and a general feeling of being unwell.
- Dermatological Symptoms: Some individuals with coeliac disease may experience dermatological symptoms, such as an itchy skin rash known as dermatitis herpetiformis. This rash usually appears on the elbows, knees, and buttocks.
- Anemia: Iron deficiency anemia is common in coeliac disease due to impaired absorption of iron in the small intestine. Anemia can cause fatigue, weakness, shortness of breath, and pale skin.
- Bone and Joint Problems: Coeliac disease can lead to decreased absorption of calcium and vitamin D, which are essential for bone health. This can result in osteoporosis (weakening of the bones), joint pain, muscle cramps, and skeletal deformities.
- Neurological Symptoms: Some individuals with coeliac disease may experience neurological symptoms, although these are less common. These symptoms can include headaches, migraines, peripheral neuropathy (tingling or numbness in the extremities), ataxia (problems with balance and coordination), and seizures.
- Fatigue and Mood Disorders: Chronic fatigue and irritability are common in individuals with coeliac disease. Mood disorders such as depression and anxiety may also occur.
It is important to note that the severity and combination of symptoms can vary greatly from person to person. Some individuals may experience mild symptoms or be asymptomatic, while others may have more severe symptoms and complications. If you suspect you may have coeliac disease or are experiencing any of these symptoms, it is important to consult a healthcare professional for proper evaluation and diagnosis.
DIAGNOSING FACTORS:
Diagnosing coeliac disease involves several factors and diagnostic tests. Here are the main steps involved in diagnosing coeliac disease:
- Medical History and Symptom Evaluation: A healthcare professional will begin by taking a detailed medical history, including a discussion of symptoms experienced. They will inquire about digestive issues, weight loss, nutritional deficiencies, dermatological symptoms, and other relevant signs or symptoms.
- Serological Tests: Blood tests are commonly used as an initial screening tool for coeliac disease. The primary blood test is the measurement of specific antibodies associated with coeliac disease, such as anti-tissue transglutaminase (anti-tTG) antibodies and anti-endomysial antibodies (EMA). Elevated levels of these antibodies indicate an immune response to gluten.
- Genetic Testing: Genetic testing may be recommended to identify the presence of certain genetic markers associated with coeliac disease, such as the HLA-DQ2 and HLA-DQ8 genes. However, it is important to note that genetic testing alone cannot confirm or exclude a diagnosis of coeliac disease, as these genetic markers are also found in individuals who do not develop the condition.
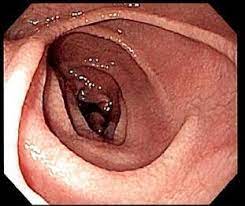
- Small Intestinal Biopsy: The definitive diagnosis of coeliac disease typically requires a small intestinal biopsy. This involves the endoscopic removal of small tissue samples from the lining of the small intestine. The biopsy samples are then examined under a microscope to assess the presence of characteristic changes associated with coeliac disease, such as villous atrophy, crypt hyperplasia, and infiltration of immune cells.
- Gluten Challenge: In certain cases, if a person is already following a gluten-free diet or has very low gluten intake, a gluten challenge may be recommended. This involves temporarily reintroducing gluten into the diet for a specific period (typically several weeks) before undergoing a small intestinal biopsy. The gluten challenge helps to ensure accurate results by provoking the characteristic changes in the small intestine that are indicative of coeliac disease.
It is essential to undergo these diagnostic procedures while still consuming gluten-containing foods, as the absence of gluten in the diet may lead to false-negative test results.
It’s important to note that diagnosis should be conducted and confirmed by a qualified healthcare professional, such as a gastroenterologist or an allergist specializing in coeliac disease. They will interpret the results of the tests in conjunction with the individual’s medical history, symptoms, and other relevant factors to make an accurate diagnosis of coeliac disease.
FOODS TO BE TAKEN:
In coeliac disease, following a strict gluten-free diet is the primary treatment and the key to managing the condition effectively. This involves avoiding all foods and drinks that contain gluten. Here is a list of foods that are safe to consume for individuals with coeliac disease:
- Naturally Gluten-Free Grains: Rice, corn, quinoa, millet, buckwheat, amaranth, sorghum, and teff are naturally gluten-free grains that can be included in the diet.
- Gluten-Free Flours and Starches: Use gluten-free flours such as rice flour, corn flour, potato flour, almond flour, coconut flour, and tapioca flour as alternatives to wheat flour. Gluten-free starches like potato starch and cornstarch can also be used for cooking and baking.
- Fruits and Vegetables: All fresh fruits and vegetables are naturally gluten-free. Include a variety of fruits and vegetables in your diet to ensure a well-rounded and balanced nutrition.
- Meat, Poultry, and Fish: Fresh meats, poultry, and fish are naturally gluten-free. However, be cautious of processed meats, sausages, and deli meats, as they may contain gluten additives or have been cross-contaminated during processing.
- Legumes and Pulses: Beans, lentils, chickpeas, and other legumes are excellent sources of protein and are naturally gluten-free.
- Dairy Products: Milk, cheese, yogurt, and butter are gluten-free, but be aware of flavored or processed dairy products that may contain gluten additives. Some individuals with coeliac disease may also have lactose intolerance, so it is important to monitor your tolerance to dairy.
- Gluten-Free Breads, Pastas, and Cereals: Look for gluten-free alternatives such as bread, pasta, and cereals made from gluten-free grains like rice, corn, or quinoa. Many stores now offer a wide variety of gluten-free options.
- Nuts and Seeds: Nuts and seeds, such as almonds, walnuts, chia seeds, flaxseeds, and sunflower seeds, are naturally gluten-free and can be incorporated into your diet for added nutrition.
- Gluten-Free Oats: Pure, uncontaminated oats are considered gluten-free and can be consumed by most individuals with coeliac disease. However, it’s important to look for oats that are specifically labeled as gluten-free to avoid cross-contamination during processing.
It is essential to carefully read food labels and be aware of potential sources of hidden gluten in processed foods, condiments, sauces, and even certain medications. Cross-contamination can occur during food preparation, so it is recommended to use separate utensils, cookware, and cutting boards for gluten-free foods.
Working with a registered dietitian who specializes in coeliac disease can provide valuable guidance and support in creating a well-balanced, gluten-free diet that meets your nutritional needs while avoiding gluten-containing foods.
LIVING WITH COELIAC DISEASE:
Managing coeliac disease requires education, careful food selection, and awareness of potential sources of hidden gluten. Reading food labels, dining out cautiously, and seeking support from healthcare professionals and support groups can greatly help individuals with coeliac disease lead a healthy and fulfilling life.
It is important to note that coeliac disease is a lifelong condition, and even small amounts of gluten can trigger symptoms and cause intestinal damage. Regular follow-up with healthcare providers is crucial to monitor the condition and ensure adequate nutritional status.
CONCLUSION:
Coeliac disease is a chronic autoimmune disorder triggered by gluten consumption. It can lead to various symptoms and complications, affecting multiple body systems. Early diagnosis, adherence to a gluten-free diet, and appropriate medical management are key to managing the disease effectively. With proper care and support, individuals with coeliac disease can lead healthy, fulfilling lives while avoiding gluten and its harmful effects on their health.