INTRODUCTION
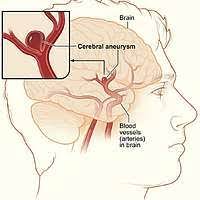
An aneurysm refers to a weakened and bulging section of an artery. It occurs when the walls of an artery become weakened, allowing it to stretch or balloon outwards. The most common type of aneurysm is an abdominal aortic aneurysm (AAA), which occurs in the part of the aorta that passes through the abdomen.
Aneurysms can also develop in other arteries, such as those in the brain (cerebral aneurysm), the heart (coronary aneurysm), or other parts of the body. If left untreated, an aneurysm can potentially rupture, leading to severe internal bleeding, which can be life-threatening.
CAUSATIVE FACTORS:
The causes of aneurysms are not always clear, but certain factors can increase the risk, including
- Weakness in the arterial wall: The primary cause of an aneurysm is a weakness in the arterial wall. This weakness can occur due to various factors, including genetic predisposition, chronic inflammation, or structural abnormalities in the blood vessel walls.
- Atherosclerosis: Atherosclerosis, which is the buildup of plaque in the arteries, can weaken the arterial walls and make them more prone to developing an aneurysm.
- High blood pressure: Persistent high blood pressure can put stress on the arterial walls, making them more susceptible to developing aneurysms.
- Smoking: Smoking damages and weakens the blood vessels, increasing the risk of aneurysm formation.
- Genetic factors: Some individuals may have an inherited predisposition to developing aneurysms. Certain genetic conditions, such as Marfan syndrome, Ehlers-Danlos syndrome, or polycystic kidney disease, can increase the risk of aneurysm formation.
- Trauma or injury: Severe trauma or injury to the blood vessels can weaken the arterial walls and lead to the development of an aneurysm.
- Infection or inflammation: Infections or inflammatory conditions, such as vasculitis, can cause damage to the arterial walls, potentially leading to the formation of aneurysms.
It’s important to note that while these factors can contribute to the development of aneurysms, not everyone with these risk factors will develop an aneurysm. Aneurysms can also occur spontaneously without any identifiable cause. Regular check-ups, managing risk factors, and seeking medical attention if you have concerns can help in the prevention or early detection of aneurysms.
SYMPTOMS OF ANEURYSM:
The symptoms of aneurysms can vary depending on the type, location, and size of the aneurysm. Here are some common symptoms associated with different types of aneurysms:
- Abdominal Aortic Aneurysm (AAA):
- Often asymptomatic and discovered incidentally during routine medical exams or imaging tests.
- In some cases, an enlarged AAA may cause a pulsating sensation in the abdomen.
- Pain in the abdomen or lower back, which may be severe or constant.
- Cerebral Aneurysm (Brain Aneurysm):
- Most cerebral aneurysms are asymptomatic until they rupture.
- Unruptured aneurysms may not cause any noticeable symptoms, or they may cause persistent or intermittent headaches.
- Ruptured aneurysms can lead to a sudden and severe headache (often described as the worst headache of one’s life), nausea, vomiting, stiff neck, blurred or double vision, sensitivity to light, seizures, loss of consciousness, and signs of a stroke, such as weakness or numbness on one side of the body or difficulty speaking.
- Thoracic Aortic Aneurysm:
- Many thoracic aortic aneurysms are asymptomatic and found incidentally.
- Symptoms may occur if the aneurysm presses against surrounding structures or if it expands rapidly, causing pain or discomfort in the chest or upper back.
- Difficulty swallowing, coughing, hoarseness, or shortness of breath can occur if the aneurysm affects the nearby structures.
- Peripheral Artery Aneurysm:
- Peripheral artery aneurysms may not cause symptoms initially.
- As the aneurysm grows, it can cause pain, throbbing, or a pulsating sensation in the affected limb.
- In some cases, the skin over the aneurysm may become discolored, develop ulcers, or feel cold to the touch.
It’s important to note that not all aneurysms cause symptoms, especially if they are small or haven’t ruptured. However, if you experience sudden and severe symptoms such as a severe headache, chest or abdominal pain, or any other concerning signs, it is essential to seek immediate medical attention, as these could indicate a potentially life-threatening condition.
DIAGNOSING FACTORS OF ANEURYSM:
The diagnosis of aneurysms involves a combination of medical history evaluation, physical examination, and various diagnostic tests. Here are some common factors used in diagnosing different types of aneurysms:
- Abdominal Aortic Aneurysm (AAA):
- Physical examination: A healthcare provider may perform a physical examination to check for a pulsating mass in the abdomen.
- Imaging tests: Ultrasound is the most common initial diagnostic test for AAA. It uses sound waves to create images of the abdominal aorta, allowing the size and location of the aneurysm to be assessed. Other imaging tests, such as CT scans or MRIs, may also be used for further evaluation.
- Cerebral Aneurysm (Brain Aneurysm):
- Imaging tests: If a cerebral aneurysm is suspected, imaging studies such as computed tomography angiography (CTA) or magnetic resonance angiography (MRA) can be performed to visualize the blood vessels in the brain and detect any abnormalities. These tests can help determine the size, location, and characteristics of the aneurysm.
- Thoracic Aortic Aneurysm:
- Imaging tests: Similar to abdominal aortic aneurysms, imaging tests such as CT scans, MRIs, or chest X-rays may be used to visualize the thoracic aorta and identify the presence, size, and location of an aneurysm.
- Peripheral Artery Aneurysm:
- Physical examination: A healthcare provider may perform a physical examination to feel for any pulsating masses or abnormal findings in the affected limb.
- Imaging tests: Ultrasound, CT scans, or MRIs may be used to evaluate the affected artery and identify the presence and characteristics of an aneurysm.
In addition to these diagnostic factors, the healthcare provider will consider the individual’s medical history, risk factors, and symptoms when making a diagnosis. It’s important to consult with a healthcare professional if you have any concerns or symptoms suggestive of an aneurysm, as they can determine the most appropriate diagnostic approach based on your specific situation.
PREVENTIVE MEASURES:
Preventive measures for different types of aneurysms may vary. However, here are some general strategies that can help reduce the risk of aneurysm formation or progression:
- Maintain a healthy lifestyle:
- Quit smoking: Smoking is a significant risk factor for aneurysm development. Quitting smoking can significantly reduce the risk.
- Eat a balanced diet: Follow a diet rich in fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit the intake of saturated and trans fats, cholesterol, and sodium.
- Exercise regularly: Engage in regular physical activity, such as aerobic exercises, to maintain a healthy weight, manage blood pressure, and improve overall cardiovascular health.
- Control blood pressure:
- Monitor blood pressure regularly and work with your healthcare provider to maintain it within a healthy range. If you have high blood pressure, follow your doctor’s recommendations for lifestyle changes and take prescribed medications as directed.
- Manage other medical conditions:
- If you have underlying medical conditions, such as high cholesterol, diabetes, or atherosclerosis, work with your healthcare provider to manage them effectively. This may involve lifestyle modifications, medications, and regular medical check-ups.
- Genetic counseling and screening:
- If you have a family history of certain genetic conditions associated with aneurysms, such as Marfan syndrome or polycystic kidney disease, consider seeking genetic counseling and screening to assess your risk and explore preventive measures.
- Regular check-ups and screenings:
- Regular medical check-ups can help monitor your overall health, detect risk factors, and identify any signs or symptoms of aneurysms early on. Follow your healthcare provider’s recommendations for screening tests or imaging studies based on your risk profile.
- Safety precautions:
- Take precautions to prevent traumatic injuries, such as using seat belts in cars, wearing appropriate protective gear during sports or physical activities, and maintaining a safe environment at home and work.
It’s important to note that preventive measures can vary depending on individual circumstances and the specific type of aneurysm. Therefore, it is recommended to consult with a healthcare professional for personalized advice and guidance regarding preventive strategies based on your specific situation.
TREATMENT OF ANEURYSM:
The treatment of aneurysms depends on several factors, including the type, size, location, and overall health of the individual. Here are some common treatment options for different types of aneurysms:
- Abdominal Aortic Aneurysm (AAA):
- Monitoring: Small AAAs that are not causing symptoms may be monitored regularly through imaging tests to track their size and growth rate.
- Surgical repair: If an AAA reaches a certain size or shows rapid growth, surgical repair may be recommended. This can involve open surgery (aneurysmectomy) to remove and replace the weakened section of the aorta with a synthetic graft or endovascular repair, where a stent graft is inserted through a minimally invasive procedure to reinforce the weakened area.
- Cerebral Aneurysm (Brain Aneurysm):
- Observation: Small unruptured cerebral aneurysms that are not causing symptoms may be monitored regularly with imaging tests to assess their stability.
- Endovascular coiling: For certain types of cerebral aneurysms, a minimally invasive procedure called endovascular coiling may be performed. It involves placing tiny platinum coils within the aneurysm to promote clotting and prevent rupture.
- Surgical clipping: In some cases, open surgery may be recommended to place a metal clip around the neck of the aneurysm to prevent blood flow into it and reduce the risk of rupture.
- Flow diverters: Flow diverting devices, such as stents, may be used to redirect blood flow away from the aneurysm and promote healing.
- Thoracic Aortic Aneurysm:
- Monitoring: Small thoracic aortic aneurysms may be monitored regularly through imaging tests to assess their size and growth.
- Surgical repair: If a thoracic aortic aneurysm reaches a certain size or shows rapid growth, surgical repair may be recommended. This can involve open surgery to replace the weakened section of the aorta with a synthetic graft or endovascular repair using stent grafts.
- Peripheral Artery Aneurysm:
- Observation: Small peripheral artery aneurysms that are not causing symptoms may be monitored regularly with imaging tests to assess their stability.
- Surgical repair: Depending on the location and size of the aneurysm, surgical repair may be considered. This can involve open surgery to remove the aneurysm and repair the affected artery or endovascular repair using stent grafts to reinforce the weakened area.
It’s important to note that treatment decisions are individualized, and the specific approach will depend on various factors, including the risk of rupture, the location of the aneurysm, the overall health of the individual, and the preference of the treating healthcare professional. Therefore, it is recommended to consult with a specialist, such as a vascular surgeon or neurosurgeon, to discuss the most suitable treatment options for your specific situation.