INTRODUCTION:
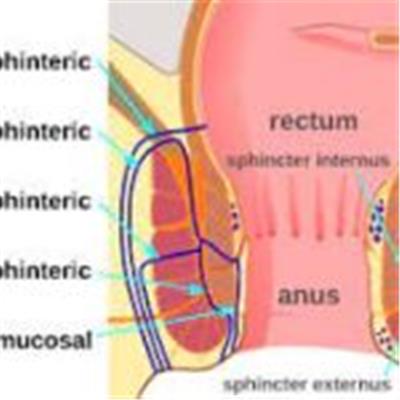
A fistula refers to an abnormal connection or passageway that forms between two organs or tissues that are not usually connected. Anal fistulas are the most well-known type, occurring when an infected anal gland forms a tunnel-like tract to the skin near the anus. Other types of fistulas can develop in various parts of the body, such as the gastrointestinal tract, urinary system, or reproductive organs.
SYMPTOMS:
- Persistent discharge: Fistulas often produce a continuous discharge of pus, mucus, or fecal matter from an opening near the affected area. The discharge may have an unpleasant odor.
- Pain and swelling: Fistulas can cause pain, swelling, and tenderness around the affected area. The pain may worsen with movement or pressure.
- Recurrent infections: Due to the abnormal connection between organs or tissues, fistulas can lead to recurrent infections in the affected area. These infections may manifest as redness, warmth, and increased pain.
- Systemic symptoms: In some cases, particularly with more extensive or complex fistulas, individuals may experience systemic symptoms such as fever, fatigue, and general malaise.
It is important to note that the symptoms can vary depending on the location and severity of the fissure or fistula. It is recommended to consult a healthcare professional for an accurate diagnosis and appropriate treatment if you experience any of these symptoms.
CAUSES OF FISTULA:
- Infection: Fistulas often develop as a result of an infection that leads to the formation of an abscess. The abscess can then erode through surrounding tissues, creating an abnormal connection or passageway.
- Inflammatory bowel disease (IBD): Crohn’s disease, in particular, is associated with a higher risk of fistula development. The chronic inflammation in the gastrointestinal tract can weaken tissues and create abnormal connections.
- Complications from surgery: Fistulas can sometimes occur as a complication of certain surgeries, such as those involving the intestines, rectum, or reproductive organs.
- Trauma or injury: Trauma or injury to the affected area, such as from a surgical procedure, radiation therapy, or accidents, can result in fistula formation.
- Other underlying conditions: Certain conditions like diverticulitis, tuberculosis, certain cancers, or conditions affecting the urinary or reproductive systems can contribute to the development of fistulas.
It’s important to note that these causes are not exhaustive, and the specific cause of a fissure or fistula can vary from person to person.
TREATMENT OF FISTULA:
- Antibiotics: If there is an active infection, antibiotics may be prescribed to control and treat the infection. This is often a temporary measure until definitive treatment can be administered.
- Surgical procedures: Surgical intervention is often necessary to treat fistulas effectively. The specific procedure will depend on the location, complexity, and severity of the fistula. Surgical options include fistulotomy (cutting open the fistula tract), seton placement (placing a thin thread-like material to keep the fistula open), advancement flaps (using nearby healthy tissue to cover the fistula), or more specialized techniques like fibrin glue or plug placement.
- Biologic therapies: In certain cases, biologic medications, such as anti-tumor necrosis factor (TNF) drugs, may be used to manage fistulas associated with conditions like Crohn’s disease by reducing inflammation and promoting healing.
- Fistula plugs: Fistula plugs made of biologic materials may be inserted into the fistula tract to close it and promote healing.
- Fistula laser closure: Laser treatment may be used in select cases to seal the fistula tract and encourage healing.
PREVENTION OF FISTULA:
- Treat underlying conditions: If you have an underlying condition such as Crohn’s disease or diverticulitis, work closely with your healthcare provider to manage and control the condition effectively. Treating and controlling the underlying disease can help reduce the risk of fistula development.
- Practice good hygiene: Maintaining proper hygiene in the affected areas can help prevent infections that may contribute to the development of fistulas. Clean the area gently and thoroughly, following your healthcare provider’s recommendations.
- Avoid self-manipulation: Do not attempt to drain or treat abscesses or infections on your own. Seek medical attention for proper evaluation and treatment to minimize the risk of complications that could lead to fistula formation.
- Follow surgical instructions: If you undergo surgery in areas at risk of fistula formation, such as the intestines or reproductive organs, follow post-operative instructions carefully to reduce the risk of complications.
- Avoid prolonged or untreated infections: Promptly seek medical attention for any infections, especially in areas susceptible to fistula development. Timely treatment can prevent the spread of infection and reduce the risk of fistula formation.
CONCLUSION:
Fistulas are abnormal passageways that develop between organs or tissues, often resulting from infections, inflammatory conditions, trauma, or complications from surgeries. They can occur in various parts of the body, such as the anal area, gastrointestinal tract, urinary system, or reproductive organs. Fistulas can cause symptoms like persistent discharge, pain, swelling, and recurrent infections.