INTRODUCTION:
Hemorrhoids are a common condition that affects many people worldwide. Also known as piles, hemorrhoids are swollen and inflamed veins in the rectum and anus. They can cause discomfort, pain, and bleeding, but in most cases, they are not a serious health concern.
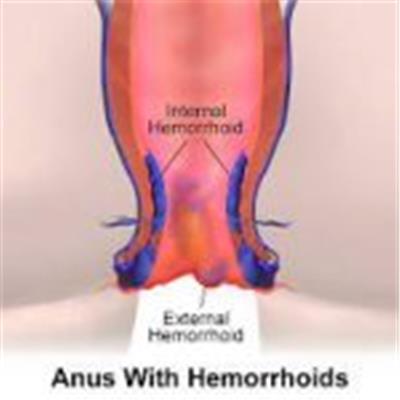
UNDERSTANDING HEMORRHOIDS:
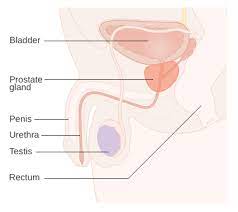
This section provides a general overview of what hemorrhoids are, including their anatomy, types (internal and external), and the factors that contribute to their development. It explains how hemorrhoids occur when the veins in the rectum or anus become swollen and inflamed.
CAUSES OF HEMORRHOIDS:
Hemorrhoids can be caused by various factors. Here are some common causes of hemorrhoids:
- Increased Pressure on the Rectal Veins: One of the primary causes of hemorrhoids is increased pressure on the veins in the rectal and anal area. This pressure can result from straining during bowel movements, which commonly occurs due to constipation or diarrhea. Prolonged sitting on the toilet, especially when straining, can also contribute to increased pressure.
- Chronic Constipation or Diarrhea: Conditions that lead to chronic constipation or diarrhea can put strain on the rectal veins and contribute to the development of hemorrhoids. Constipation can cause hard and dry stools that require increased straining during bowel movements, while diarrhea can lead to frequent loose stools that irritate the rectal area.
- Pregnancy: Hemorrhoids are a common occurrence during pregnancy. The growing uterus exerts pressure on the rectal veins, and hormonal changes can contribute to the development of hemorrhoids. Additionally, the strain during childbirth can further aggravate or cause hemorrhoids.
- Obesity: Being overweight or obese increases the likelihood of developing hemorrhoids. Excess weight puts additional pressure on the rectal veins, making them more susceptible to swelling and inflammation.
- Sedentary Lifestyle: Lack of physical activity and prolonged periods of sitting or standing can contribute to the development of hemorrhoids. Regular physical activity helps promote healthy bowel movements and reduces the risk of constipation, which can alleviate strain on the rectal veins.
- Aging: The risk of developing hemorrhoids increases with age. As people get older, the tissues supporting the veins in the rectum and anus may weaken, making them more prone to swelling and the development of hemorrhoids.
- Heredity: There may be a genetic predisposition to hemorrhoids, meaning that individuals with a family history of hemorrhoids are more likely to develop them.
It’s important to note that while these factors can increase the risk of developing hemorrhoids, they do not guarantee their occurrence. Lifestyle modifications, such as maintaining a healthy diet, staying physically active, and practicing good bathroom habits, can help reduce the risk of hemorrhoids. If you are experiencing symptoms of hemorrhoids or are concerned about your condition, it is advisable to consult a healthcare professional for an accurate diagnosis and appropriate treatment.
SYMPTOMS:
Hemorrhoids can cause a variety of symptoms, which can vary depending on the type and severity of the condition. Here are some common symptoms associated with hemorrhoids:
- Rectal Bleeding: One of the most common symptoms of hemorrhoids is rectal bleeding. This typically presents as bright red blood on the toilet paper, in the toilet bowl, or coating the stool after a bowel movement. The bleeding is usually painless and may be intermittent.
- Itching and Irritation: Hemorrhoids can cause itching and irritation in the anal area. This itching may be persistent or intermittent and can be quite bothersome. Scratching the affected area can further exacerbate the irritation.
- Pain or Discomfort: External hemorrhoids, which develop under the skin around the anus, can cause pain or discomfort. The pain may worsen during bowel movements or when sitting for extended periods. Internal hemorrhoids, on the other hand, are typically painless unless they become prolapsed or thrombosed (blood clot forms inside).
- Swelling and Lump Formation: External hemorrhoids may cause visible swelling around the anus. These swollen veins can form a lump or a firm, tender mass that can be felt or seen. Internal hemorrhoids, when prolapsed, can also protrude from the anus and appear as moist, pink tissue.
- Bowel Movement Changes: Hemorrhoids can affect bowel movements. Individuals with hemorrhoids may experience difficulty or pain during bowel movements due to the swollen veins and the associated inflammation. This can sometimes lead to a feeling of incomplete evacuation.
- Mucus Discharge: Some individuals with hemorrhoids may experience a mucus discharge from the anus. This discharge can cause a feeling of dampness or moisture in the anal area.
It’s important to note that these symptoms can also be indicative of other conditions, such as anal fissures or more serious colorectal issues. If you experience rectal bleeding or persistent symptoms, it is recommended to consult a healthcare professional for proper evaluation and diagnosis. They can provide an accurate diagnosis and recommend appropriate treatment options based on your specific condition.
DIAGNOSIS AND EVALUATION:
Diagnosing hemorrhoids typically involves a combination of a medical history review, physical examination, and in some cases, additional tests. Here’s an overview of the diagnostic process for hemorrhoids:
- Medical History Review: Your healthcare provider will ask you about your symptoms, including any pain, itching, bleeding, or changes in bowel movements. They will inquire about your medical history, including any previous occurrences of hemorrhoids, relevant family history, and any chronic conditions that may contribute to the development of hemorrhoids.
- Physical Examination: During a physical examination, your healthcare provider will visually inspect the anal area to look for signs of hemorrhoids, such as swelling, inflammation, or external lumps. They may also perform a digital rectal examination, which involves inserting a gloved, lubricated finger into the rectum to assess for internal hemorrhoids or other abnormalities.
- Additional Tests:
- Anoscopy: If internal hemorrhoids are suspected, your healthcare provider may perform an anoscopy. This involves using a small, lighted tube called an anoscope to visualize the inside of the anus and lower rectum.
- Colonoscopy or Sigmoidoscopy: In cases where symptoms are persistent, severe, or if there is concern about other underlying conditions, your healthcare provider may recommend a colonoscopy or sigmoidoscopy. These procedures involve using a flexible tube with a camera to examine the entire colon or the lower part of the colon and rectum, respectively.
It’s important to note that rectal bleeding and other symptoms associated with hemorrhoids can also be indicative of other conditions, such as anal fissures, inflammatory bowel disease, or colorectal cancer. Therefore, it’s crucial to consult a healthcare professional for an accurate diagnosis. They will be able to differentiate between hemorrhoids and other potential causes of your symptoms and recommend appropriate treatment options based on the findings.
If you’re experiencing rectal bleeding or persistent symptoms, it’s advisable to seek medical attention to ensure a proper evaluation and diagnosis.
TREATMENT:
The treatment of hemorrhoids depends on the severity and specific symptoms experienced. In many cases, conservative measures and self-care techniques are sufficient to alleviate symptoms and promote healing. However, for more severe or persistent cases, medical interventions may be necessary. Here are various treatment options for hemorrhoids:
- Self-Care and Lifestyle Modifications:
- Increasing fiber intake: Consuming a high-fiber diet can soften stools and make them easier to pass, reducing the strain on hemorrhoids. Good sources of fiber include fruits, vegetables, whole grains, and legumes.
- Adequate hydration: Drinking plenty of water helps maintain soft stools and prevents constipation.
- Avoiding straining: Straining during bowel movements should be avoided. If necessary, a stool softener or fiber supplement may be recommended.
- Sitz baths: Soaking the anal area in warm water for 10 to 15 minutes several times a day can help relieve symptoms and promote healing.
- Good hygiene: Keeping the anal area clean and dry after bowel movements, using moist wipes or gentle patting instead of harsh wiping, can help prevent further irritation.
- Topical Medications:
- Over-the-counter creams, ointments, or suppositories containing hydrocortisone or witch hazel can help reduce itching, inflammation, and discomfort associated with hemorrhoids.
- Procedures and Interventions:
- Rubber band ligation: A common outpatient procedure where a rubber band is placed around the base of an internal hemorrhoid to cut off its blood supply, causing it to wither and fall off.
- Sclerotherapy: Injection of a chemical solution into the hemorrhoid to shrink and reduce its size.
- Infrared coagulation: Using heat to coagulate the blood vessels within the hemorrhoid, causing it to shrink.
- Hemorrhoidectomy: Surgical removal of hemorrhoids, usually performed for severe cases or when other treatments have been ineffective. This procedure may be associated with more significant discomfort during recovery.
- Hemorrhoidal Stapling:
- This procedure, known as stapled hemorrhoidopexy or procedure for prolapse and hemorrhoids (PPH), involves using a special stapling device to remove excess tissue and reposition the remaining hemorrhoidal tissue to its normal position.
It’s important to consult a healthcare professional to determine the most appropriate treatment approach for your specific condition. They can assess the severity of your hemorrhoids and recommend the best course of action, taking into consideration your medical history and individual circumstances.
PREVENTION AND SELFCARE:
It covers strategies such as maintaining a high-fiber diet, staying hydrated, avoiding prolonged sitting or straining, regular exercise, and practicing good bathroom habits.
- High-Fiber Diet: Consuming a diet rich in fiber helps maintain regular bowel movements and prevents constipation. Include plenty of fruits, vegetables, whole grains, and legumes in your diet. Aim for 25-30 grams of fiber per day.
- Stay Hydrated: Drinking an adequate amount of water throughout the day helps keep stools soft and easier to pass. Aim for at least 8 glasses (64 ounces) of water daily, or adjust based on your body’s needs.
- Regular Exercise: Engaging in regular physical activity promotes healthy bowel movements and prevents constipation. Try to incorporate moderate exercise, such as walking, jogging, or swimming, into your routine.
- Avoid Straining: Avoid straining during bowel movements, as it can increase pressure on the rectal veins. Take your time in the bathroom, and if needed, use a stool softener or fiber supplement to prevent constipation.
- Proper Bathroom Habits:
- Don’t delay or ignore the urge to have a bowel movement.
- Avoid excessive straining or prolonged sitting on the toilet.
- Use moist wipes or gentle patting with soft toilet paper instead of harsh wiping.
- Clean the anal area gently and thoroughly after bowel movements.
- Maintain a Healthy Weight: Maintaining a healthy weight reduces the strain on the rectal veins and decreases the risk of developing hemorrhoids. Incorporate a balanced diet and regular exercise to manage your weight effectively.
- Take Breaks from Prolonged Sitting: If your work or lifestyle involves long periods of sitting, take regular breaks to stand and move around. This helps improve blood circulation and reduces pressure on the rectal veins.
- Avoid Heavy Lifting: Heavy lifting can increase intra-abdominal pressure and strain the rectal veins. If you need to lift something heavy, use proper lifting techniques and avoid holding your breath while doing so.
- Practice Good Posture: Maintain good posture to prevent unnecessary pressure on the rectal veins. Sit and stand with an upright posture, avoiding excessive slouching.
- Manage Chronic Conditions: If you have chronic conditions such as constipation or diarrhea, work with your healthcare provider to manage these conditions effectively and reduce the risk of hemorrhoids.
By adopting these preventive measures, you can reduce the likelihood of developing hemorrhoids or minimize their recurrence. If you have any concerns or experience persistent symptoms, consult a healthcare professional for appropriate advice.