INTRODUCTION:
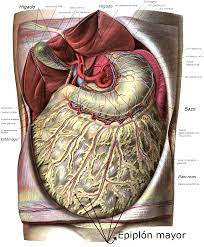
Peritonitis is a serious medical condition characterized by the inflammation of the peritoneum, which is the thin tissue lining the inner wall of the abdomen and covering the organs within it. This condition requires immediate medical attention as it can lead to severe complications if left untreated.
CAUSES:
Peritonitis most commonly occurs due to an infection, often resulting from the spread of bacteria or fungi into the peritoneum. The infection can arise from various sources, including:
- Ruptured Appendix: When the appendix bursts, it releases bacteria into the abdominal cavity, leading to peritonitis.
- Abdominal Trauma: Blunt or penetrating trauma to the abdomen can cause a rupture in the organs, allowing bacteria to enter the peritoneum.
- Peritoneal Dialysis: People undergoing peritoneal dialysis for kidney failure are at risk of developing peritonitis due to the introduction of bacteria during the procedure.
- Gastrointestinal Perforation: Conditions such as gastric ulcers, diverticulitis, or a perforated bowel can allow bacteria to enter the peritoneum.
- Pelvic Inflammatory Disease (PID): In women, untreated PID can spread bacteria from the reproductive organs to the peritoneum.
SYMPTOMS:
Symptoms of peritonitis can vary depending on the underlying cause and the severity of the condition. Here are some common symptoms associated with peritonitis:
- Abdominal Pain: One of the hallmark symptoms of peritonitis is severe abdominal pain. The pain may be localized or generalized and is often described as a sharp, constant, or cramping sensation. It typically worsens with movement or pressure on the abdomen.
- Abdominal Tenderness: The abdomen may feel tender to touch, and even gentle pressure can cause significant discomfort.
- Abdominal Distention: Peritonitis can lead to abdominal bloating and distention, causing the abdomen to appear swollen or enlarged.
- Fever and Chills: Infection-related peritonitis is often accompanied by fever and chills. The body’s immune response to the infection can cause an elevated body temperature.
- Nausea and Vomiting: Many individuals with peritonitis experience nausea and may vomit. This can be a result of the underlying infection or inflammation in the abdominal cavity.
- Loss of Appetite: Peritonitis can cause a decreased desire to eat, leading to a loss of appetite.
- Fatigue and Weakness: The inflammatory response and the body’s effort to fight the infection can result in feelings of fatigue and weakness.
- Elevated Heart Rate: Peritonitis can cause an increased heart rate (tachycardia) as the body tries to compensate for the infection and inflammation.
- Reduced Urine Output: In severe cases, peritonitis may affect kidney function, leading to decreased urine output.
It’s important to note that these symptoms can also be present in other abdominal conditions, so it is crucial to consult a healthcare professional for an accurate diagnosis if you experience any of these symptoms. Early detection and treatment of peritonitis are essential to prevent complications and promote recovery.
DIAGNOSING FACTORS:
When diagnosing peritonitis, healthcare professionals consider various factors to determine the presence of the condition and its underlying cause. Here are some key factors and diagnostic measures used in the diagnosis of peritonitis:
- Medical History and Physical Examination: A thorough review of the patient’s medical history, including any previous abdominal surgeries, infections, or conditions, can provide important clues. During a physical examination, the healthcare professional may assess the abdomen for tenderness, distention, and signs of infection.
- Symptom Assessment: The patient’s reported symptoms, such as severe abdominal pain, tenderness, fever, nausea, vomiting, and changes in appetite, provide valuable information for the diagnostic process.
- Laboratory Tests:
- Complete Blood Count (CBC): A CBC can help identify an elevated white blood cell count (leukocytosis), which indicates an immune response to infection.
- Blood Culture: Blood samples may be collected to identify the presence of bacteria or fungi in the bloodstream, which can indicate an underlying infection.
- Inflammatory Markers: Measurement of inflammatory markers, such as C-reactive protein (CRP) and erythrocyte sedimentation rate (ESR), can help assess the severity of inflammation.
- Imaging Studies:
- X-rays: Abdominal X-rays may be performed to identify signs of bowel obstruction, perforation, or the presence of free air in the abdominal cavity.
- Ultrasound: Abdominal ultrasound can help visualize the organs and detect abnormalities, such as abscesses or fluid collections.
- Computed Tomography (CT) Scan: CT scans provide detailed cross-sectional images of the abdomen, helping to identify the cause of peritonitis, such as perforations, abscesses, or inflammation.
- Peritoneal Fluid Analysis: In some cases, a sample of peritoneal fluid may be collected through a procedure called paracentesis. The fluid is analyzed for the presence of bacteria, white blood cells, and other indicators of infection or inflammation.
- Source Identification: If peritonitis is suspected, efforts are made to identify the underlying cause. This may involve additional tests or procedures, such as an endoscopy, colonoscopy, or exploratory laparotomy, to visualize and evaluate the organs directly.
The combination of medical history, physical examination, laboratory tests, imaging studies, and source identification helps healthcare professionals diagnose peritonitis accurately and determine the most appropriate treatment approach. Swift and accurate diagnosis is crucial for initiating timely treatment and preventing complications associated with peritonitis.
TREATMENT:
Treatment for peritonitis typically involves a combination of antibiotics to combat the infection, surgical intervention to address the underlying cause, and supportive care to manage symptoms. The specific treatment approach may vary depending on the individual case.
- Antibiotics: Broad-spectrum antibiotics are administered intravenously to target the infection. The choice of antibiotics may be adjusted based on the results of culture and sensitivity tests.
- Surgery: Surgical intervention is often necessary to repair any perforations or remove infected tissues, such as in the case of a ruptured appendix or gastrointestinal perforation.
- Supportive Care: Pain management, intravenous fluids, and nutritional support may be provided to stabilize the patient and support their recovery.
CONCLUSION:
Peritonitis is a serious condition that requires urgent medical attention. Timely diagnosis and appropriate treatment, including antibiotics and surgical intervention, are vital for a successful recovery. If you experience persistent abdominal pain, fever, or other symptoms suggestive of peritonitis, it is crucial to seek immediate medical care to prevent complications and improve outcomes.