INTRODUCTION:
Guillain-Barré Syndrome (GBS) is a rare and potentially life-threatening neurological disorder that affects the peripheral nervous system. Named after French physicians Georges Guillain and Jean Alexandre Barré, who first described the condition in 1916, GBS is characterized by the rapid onset of muscle weakness, numbness, and in severe cases, paralysis. Although relatively uncommon, understanding the causes, symptoms, diagnosis, and treatment of Guillain-Barré Syndrome is crucial in providing appropriate medical care and support to those affected by this challenging condition.
CAUSES AND RISK FACTORS:
The exact cause of GBS is not fully understood, but it is often preceded by an infection, typically a respiratory or gastrointestinal infection caused by certain bacteria or viruses. The most commonly associated pathogens include Campylobacter jejuni, Epstein-Barr virus, cytomegalovirus, and the bacteria responsible for respiratory infections such as Haemophilus influenzae and Mycoplasma pneumoniae. It is important to note that GBS is not contagious.
The immune response triggered by these infections is believed to play a key role in the development of Guillain-Barré Syndrome. In some cases, the immune system mistakenly attacks the peripheral nerves, leading to inflammation and damage.
SYMPTOMS AND PROGRESSION:
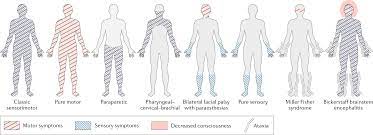
Guillain-Barré Syndrome (GBS) is characterized by a rapid onset of symptoms that typically begin in the legs and can progress upwards. The specific symptoms can vary among individuals, but here are some common signs and symptoms of GBS:
- Muscle Weakness: GBS often starts with weakness in the legs, which can gradually spread to the arms and upper body. The weakness is usually symmetrical, affecting both sides of the body.
- Tingling Sensations: Many individuals with GBS experience tingling or a “pins and needles” sensation in their extremities. This sensation may be accompanied by numbness.
- Loss of Reflexes: Reflexes, such as the knee-jerk reflex, may be diminished or absent. This is due to the damage to the nerves involved in reflex responses.
- Sensory Changes: GBS can cause sensory disturbances, including heightened sensitivity, numbness, or pain in the affected areas.
- Muscle Pain: Some individuals may experience muscle pain or cramps, which can be a precursor to weakness.
- Difficulty with Coordination: GBS can affect coordination and balance, leading to problems with walking or performing fine motor tasks.
- Autonomic Dysfunction: In severe cases, GBS can affect the autonomic nervous system, which controls involuntary bodily functions. This can result in fluctuations in blood pressure, heart rate abnormalities, sweating abnormalities, and bladder or bowel dysfunction.
- Breathing Difficulties: Rarely, GBS can lead to respiratory muscle weakness, causing difficulty in breathing. It is important to seek immediate medical attention if experiencing any respiratory symptoms.
The progression of GBS can vary among individuals. In some cases, the symptoms may reach their peak within a few weeks, while in others, they may progress over several months. Although rare, respiratory failure and severe muscle weakness may require immediate medical intervention.
DIAGNOSIS AND TREATMENT:
The diagnosis of Guillain-Barré Syndrome (GBS) involves a combination of medical history, physical examination, and specific diagnostic tests. Here are the key factors used in diagnosing GBS:
- Medical History: The doctor will inquire about the onset and progression of symptoms, including any recent infections or illnesses that may have preceded the development of GBS. Information about any relevant vaccinations, medications, or exposure to toxins will also be considered.
- Physical Examination: The healthcare provider will conduct a thorough neurological examination to assess muscle strength, reflexes, coordination, sensation, and other neurological functions. They will look for signs of muscle weakness, diminished reflexes, sensory abnormalities, and autonomic dysfunction.
- Nerve Conduction Studies (NCS): NCS involve placing electrodes on the skin to measure the speed and strength of electrical signals as they travel along the nerves. In GBS, nerve conduction studies typically show a characteristic pattern of nerve damage and slowing of nerve signals.
- Lumbar Puncture (Spinal Tap): A lumbar puncture involves inserting a needle into the lower back to collect a sample of cerebrospinal fluid (CSF). CSF analysis can help detect elevated levels of proteins and the presence of immune cells, which are indicative of the inflammatory process associated with GBS.
- Electromyography (EMG): EMG involves inserting a needle electrode into muscles to evaluate their electrical activity. Abnormal EMG findings, such as increased muscle activity at rest or reduced activity during voluntary movement, can provide evidence of nerve damage in GBS.
- Blood Tests: Blood tests may be conducted to rule out other potential causes of symptoms and to check for specific antibodies associated with GBS, such as antibodies to Campylobacter jejuni, which is a common bacterial trigger for the syndrome.
It is important to note that the diagnosis of GBS can be complex, and the specific tests used may vary depending on the individual case. Sometimes, additional imaging studies, such as magnetic resonance imaging (MRI), may be performed to rule out other conditions that may mimic GBS.
Prompt and accurate diagnosis is crucial for timely treatment and management of GBS. If you suspect GBS or experience symptoms consistent with the syndrome, it is important to consult a healthcare professional for proper evaluation and diagnosis.
Treatment for GBS primarily focuses on managing symptoms, providing supportive care, and preventing complications. Hospitalization is often necessary to closely monitor the patient’s condition. Intravenous immunoglobulin (IVIG) therapy and plasma exchange (plasmapheresis) are commonly used to reduce the severity and duration of symptoms by modulating the immune response. Physical therapy and rehabilitation are also essential for recovery and restoring muscle strength and function.
PROGNOSIS AND RECOVERY:
The prognosis for Guillain-Barré Syndrome varies widely. While some individuals experience a full recovery, others may have residual weakness or sensory deficits. The recovery period can range from weeks to months, and in some cases, even years. Rehabilitation programs, including physical therapy, occupational therapy, and speech therapy, can significantly aid in the recovery process and improve quality of life.
CONCLUSION:
Guillain-Barré Syndrome is a rare neurological disorder characterized by muscle weakness, numbness, and in severe cases, paralysis. Although the exact cause is not fully understood, it is often preceded by an infection that triggers an immune response leading to nerve damage. Early diagnosis, supportive care, and appropriate treatment are crucial for managing GBS effectively and minimizing potential complications. Through medical intervention and rehabilitative therapies, individuals with Guillain-Barré Syndrome can often regain their strength and resume their normal lives with time and dedication.