INTRODUCTION:
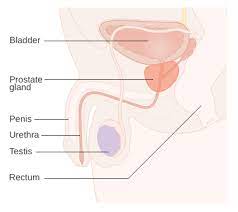
Prostate cancer is a type of cancer that develops in the prostate gland, which is a small walnut-shaped gland in males that produces seminal fluid. It is one of the most common cancers among men.
CAUSES:
The exact cause of prostate cancer is unknown, but certain risk factors can increase the likelihood of developing the disease. These risk factors include age (prostate cancer is more common in older men), family history of prostate cancer, certain genetic mutations, race (African-American men have a higher risk), and certain lifestyle factors such as a high-fat diet.
SYMPTOMS:
The symptoms of prostate cancer can vary among individuals, and in the early stages, prostate cancer may not cause any noticeable symptoms. However, as the cancer progresses, the following symptoms may occur:
- Urinary Symptoms:
- Frequent urination, particularly during the night (nocturia)
- Difficulty starting or stopping urination
- Weak or interrupted urine flow
- Inability to empty the bladder completely
- Urgency to urinate
- Blood in the urine (hematuria)
- Sexual Symptoms:
- Erectile dysfunction (difficulty achieving or maintaining an erection)
- Pain or discomfort during ejaculation
- Decreased force in the stream of semen
- Other Symptoms:
- Blood in the semen (hematospermia)
- Pain or discomfort in the pelvic area, lower back, hips, or upper thighs
- Bone pain, especially in advanced stages if cancer has spread to the bones
- Unintentional weight loss
- Fatigue or weakness
It’s important to note that these symptoms can also be caused by other non-cancerous conditions such as benign prostatic hyperplasia (BPH), urinary tract infections, or prostatitis. Therefore, experiencing these symptoms does not necessarily mean a person has prostate cancer. However, if you are experiencing any persistent or concerning symptoms, it is recommended to consult a healthcare professional for further evaluation and appropriate testing.
Additionally, it’s worth noting that routine prostate cancer screening, such as the prostate-specific antigen (PSA) test, can help detect the cancer before symptoms appear. Regular check-ups and discussions with your healthcare provider about the potential benefits and risks of screening are important, especially for individuals with risk factors or a family history of prostate cancer.
DIFFERENT DIAGNOSING FACTORS:
Certainly! When diagnosing prostate cancer, healthcare professionals consider several factors to make an accurate assessment. Here are the key elements involved in the diagnostic process:
- Medical History: The healthcare provider will start by taking a detailed medical history, including any symptoms the patient may be experiencing, family history of prostate cancer or other cancers, and information about any previous medical conditions or treatments.
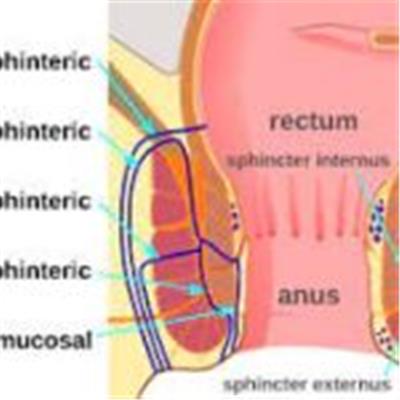
- Physical Examination: A physical examination, including a digital rectal examination (DRE), is commonly performed to check for any abnormalities in the prostate gland. During a DRE, the doctor inserts a gloved, lubricated finger into the rectum to feel the prostate for lumps, hard areas, or other abnormalities.
- Prostate-Specific Antigen (PSA) Test: The PSA test measures the level of prostate-specific antigen, a protein produced by both normal and cancerous prostate cells, in the blood. Elevated PSA levels can be an indication of prostate cancer, although other factors such as age, prostate size, and certain medications can also affect PSA levels. If the PSA levels are elevated, further tests may be recommended.
- Imaging Tests: Various imaging tests may be used to evaluate the prostate and surrounding tissues. These may include:
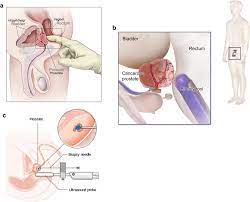
- Transrectal Ultrasound (TRUS): A probe inserted into the rectum emits sound waves that create images of the prostate gland.
- Magnetic Resonance Imaging (MRI): An MRI scan provides detailed images of the prostate, allowing doctors to assess the size, shape, and potential spread of cancer.
- Computed Tomography (CT) Scan: CT scans may be used to examine the pelvic region and detect any spread of cancer to nearby lymph nodes or other organs.
- Biopsy: A prostate biopsy is considered the definitive method to confirm the presence of cancer. During a biopsy, a small tissue sample is taken from the prostate gland using a thin needle. The sample is then examined under a microscope by a pathologist to determine if cancer cells are present and to assess the aggressiveness of the cancer.
- Transrectal Ultrasound-Guided Biopsy: This is the most common biopsy technique, where an ultrasound probe guides the placement of the biopsy needle into the prostate through the rectum.
- Transperineal Biopsy: In some cases, a biopsy may be performed through the perineum (the area between the scrotum and anus), using either an ultrasound or MRI for guidance.
- Gleason Score: After a biopsy, the pathologist assigns a Gleason score to the cancer cells. The Gleason score indicates the aggressiveness or grade of the cancer and helps guide treatment decisions. It ranges from 2 to 10, with higher scores indicating more aggressive cancer cells.
- Combining these factors, the cancer is assigned a stage ranging from I to IV, with higher stages indicating more advanced cancer.
- Tumor (T) stage: Describes the size and extent of the primary tumor within the prostate gland.
- Node (N) stage: Indicates whether cancer has spread to nearby lymph nodes.
- Metastasis (M) stage: Determines if cancer has spread to other parts of the body.
The diagnostic process for prostate cancer involves a combination of these factors to provide a comprehensive understanding of the disease. It’s important to consult with a healthcare professional who can guide you through the diagnostic process and provide personalized recommendations based on your specific situation.
TREATMENT:
The treatment options for prostate cancer depend on various factors, including the stage of cancer, the aggressiveness of the tumor, the overall health of the patient, and the patient’s preferences. Common treatment approaches include:
- Active surveillance: For slow-growing tumors, the doctor may recommend regular monitoring without immediate treatment, especially in older patients or those with other health conditions.
- Surgery: Surgical options include radical prostatectomy, where the entire prostate gland is removed, or a transurethral resection of the prostate (TURP) for relieving symptoms in advanced cases.
- Radiation therapy: This treatment uses high-energy rays to kill cancer cells. It can be delivered externally (external beam radiation therapy) or internally (brachytherapy).
- Hormone therapy: Prostate cancer is often hormone-sensitive, so hormone therapy is used to reduce the levels of testosterone or block its effects on cancer cells.
- Chemotherapy: It may be recommended for advanced cases or when the cancer has spread to other parts of the body.
- Immunotherapy: Some newer treatment options involve boosting the immune system to fight cancer cells more effectively.
It’s important to consult with healthcare professionals, such as oncologists or urologists, who can provide personalized advice and discuss the most suitable treatment options based on an individual’s specific case.
CONCLUSION:
In conclusion, prostate cancer is a common form of cancer that affects the prostate gland in males. It typically develops in older men and can be influenced by various risk factors such as age, family history, genetic mutations, race, and lifestyle choices.
Regular screenings and discussions with healthcare providers regarding risk factors, symptoms, and appropriate testing are essential for early detection and effective management of prostate cancer. If you have concerns about prostate cancer or are experiencing any related symptoms, it is best to consult a qualified healthcare professional for proper evaluation and guidance.