INTRODUCTION:
Ehlers-Danlos syndrome (EDS) is a group of genetic disorders that affect the connective tissues in the body. Connective tissues provide support, structure, and elasticity to various organs, skin, joints, and blood vessels. EDS is caused by abnormalities in the production, structure, or processing of collagen, which is the main protein component of connective tissues.
There are several types of Ehlers-Danlos syndrome, each with its own set of symptoms and characteristics. The most common types include:
- Classical EDS (cEDS): Characterized by hyperextensible (stretchy) skin, joint hypermobility, and increased susceptibility to skin bruising and scarring. It may also involve joint instability and complications such as hernias or organ prolapse.
- Hypermobility EDS (hEDS): The primary feature is joint hypermobility, which can lead to joint pain, dislocations, and chronic musculoskeletal symptoms. Other symptoms may include soft, velvety skin and gastrointestinal issues.
- Vascular EDS (vEDS): This is the most severe and potentially life-threatening form of EDS. It is characterized by thin, translucent skin, fragile blood vessels, and organ rupture. Individuals with vEDS are at high risk of arterial or organ rupture, which can be life-threatening.
- Kyphoscoliotic EDS (kEDS): Associated with severe muscle weakness, joint deformities, scoliosis, and fragile connective tissues. Individuals with kEDS may also experience respiratory complications and increased risk of eye and hearing problems.
- Other rare types: There are several other rare types of EDS, including dermatosparaxis EDS, arthrochalasia EDS, and others. Each type has distinct features and associated genetic mutations.
Diagnosis of Ehlers-Danlos syndrome typically involves a thorough evaluation of medical history, physical examination, assessment of symptoms, and genetic testing. Management of EDS is focused on addressing specific symptoms and complications. Treatment may include physical therapy to strengthen muscles and stabilize joints, pain management strategies, bracing or orthotics for joint support, and regular monitoring for potential complications.
It’s important for individuals with Ehlers-Danlos syndrome to work closely with healthcare professionals experienced in managing the condition to receive appropriate care, support, and guidance for symptom management and overall well-being.
SYMPTOMS:

Ehlers-Danlos syndrome (EDS) is a group of genetic disorders that affect the connective tissues in the body. The symptoms of EDS can vary depending on the specific type of EDS a person has and the severity of their condition. Here are some common symptoms associated with EDS:
- Skin symptoms:
- Hyperextensibility: The skin can be excessively stretchy and elastic, with the ability to stretch further than normal.
- Fragile skin: The skin may be fragile and prone to tearing, bruising, or scarring easily.
- Easy bruising: Individuals with EDS may experience easy bruising or the formation of bruises with minimal trauma.
- Thin or translucent skin: The skin may appear thin or translucent, allowing blood vessels or underlying structures to be visible.
- Joint and musculoskeletal symptoms:
- Joint hypermobility: Joints can move beyond the normal range of motion, leading to increased flexibility.
- Joint instability: The joints may be unstable, prone to dislocations or subluxations (partial dislocations).
- Joint pain: Chronic joint pain is common, often associated with joint hypermobility or instability.
- Muscle weakness: Some types of EDS can involve muscle weakness or poor muscle tone.
- Vascular symptoms (in certain types of EDS, particularly vascular EDS):
- Fragile blood vessels: The blood vessels may be weak and prone to rupture or aneurysm formation.
- Easy bruising or bleeding: Individuals with vascular EDS may experience easy bruising or prolonged bleeding due to fragile blood vessels.
- Gastrointestinal symptoms:
- Gastrointestinal dysmotility: Some individuals with EDS may experience abnormalities in the movement of the digestive tract, leading to symptoms such as chronic constipation or gastroesophageal reflux.
- Hernias: EDS can increase the risk of developing hernias, such as inguinal or hiatal hernias.
- Other symptoms:
- Chronic pain: Many individuals with EDS experience chronic pain, which may be musculoskeletal or widespread.
- Fatigue: Fatigue or generalized weakness is commonly reported.
- Autonomic dysfunction: Some types of EDS can involve dysfunction of the autonomic nervous system, leading to symptoms such as orthostatic intolerance (dizziness upon standing) or gastrointestinal dysmotility.
It’s important to note that symptoms can vary significantly among individuals with EDS, even within the same type. Some individuals may have mild symptoms, while others may experience more severe manifestations of the condition. If you suspect you or someone you know may have EDS, it’s important to consult with a healthcare professional for a proper evaluation, diagnosis, and management plan.
MANAGEMENT:
The management of Ehlers-Danlos syndrome (EDS) aims to alleviate symptoms, prevent complications, and improve overall quality of life. While there is no cure for EDS, a comprehensive approach to management typically involves a combination of strategies. Here are some key aspects of managing EDS:
- Medical care coordination: It is important to establish a care team that includes healthcare professionals familiar with EDS, such as geneticists, rheumatologists, orthopedic specialists, and physical therapists. Regular communication and coordination among these professionals are crucial.
- Symptom-specific management:
- Joint instability and pain: Physical therapy and exercise programs designed to strengthen muscles and stabilize joints can help manage joint instability and alleviate pain. Assistive devices such as braces or orthotics may provide additional support.
- Skin-related issues: Gentle skin care, including moisturizing and avoiding activities that may cause excessive stretching or trauma to the skin, can help minimize symptoms such as skin fragility, easy bruising, or scarring.
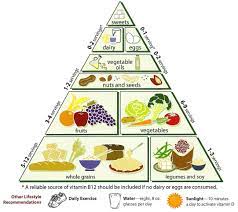
- Gastrointestinal symptoms: Dietary modifications, including a high-fiber diet and adequate hydration, may help manage gastrointestinal issues such as constipation. Medications or interventions may be considered for specific symptoms under the guidance of a gastroenterologist.
- Pain management: Chronic pain management may involve a multimodal approach, including physical therapy, medication management, relaxation techniques, and alternative therapies such as acupuncture or massage.
- Cardiovascular monitoring: Regular cardiovascular evaluations are important to monitor for potential complications associated with specific types of EDS, especially vascular EDS. Regular check-ups, imaging studies, and collaboration with a cardiologist can help detect and manage cardiovascular issues.
- Psychological support: Living with a chronic condition like EDS can impact mental health. Supportive counseling, support groups, and psychological interventions can provide emotional support, coping strategies, and help manage the psychological impact of the condition.
- Lifestyle modifications:
- Exercise and physical activity: Engaging in regular low-impact exercise programs, under the guidance of a physical therapist, can help improve muscle tone, joint stability, and overall physical function.
- Joint protection: Adopting proper body mechanics and techniques to protect joints during daily activities can help minimize the risk of joint injuries and reduce pain.
- Avoiding high-risk activities: Individuals with EDS should avoid activities that can pose a higher risk of injury, such as high-impact sports or activities that put excessive strain on the joints or skin.
- Genetic counseling and family planning: Genetic counseling is beneficial for individuals with EDS and their families to understand the inheritance pattern, discuss family planning options, and address any concerns or questions.
Management of EDS should be individualized based on the specific type and severity of symptoms. It is important for individuals with EDS to maintain open communication with their healthcare team, adhere to recommended treatment plans, and seek medical advice when needed. Regular follow-ups and monitoring are essential for optimizing care and addressing any changes or complications that may arise.
It’s important for individuals with EDS to work closely with a multidisciplinary team of healthcare professionals experienced in managing the condition. The treatment approach should be personalized based on individual needs, symptom severity, and specific type of EDS. Regular follow-ups and communication with healthcare providers are crucial for ongoing management and support.
TREATMENT:
The treatment of Ehlers-Danlos syndrome (EDS) focuses on managing symptoms, preventing complications, and improving overall quality of life. While there is no cure for EDS, various treatment strategies can help individuals with the condition. Here are some common approaches to the treatment of EDS:
- Physical therapy and exercise: Physical therapy plays a crucial role in managing EDS by focusing on strengthening muscles, improving joint stability, and promoting proper body mechanics. Therapeutic exercises and techniques can help reduce pain, improve mobility, and prevent injuries.
- Pain management: Chronic pain is a common symptom of EDS, and pain management strategies may include a combination of medications, physical therapy, and alternative therapies such as acupuncture, massage, or transcutaneous electrical nerve stimulation (TENS).
- Joint protection and orthopedic interventions: Assistive devices like braces, splints, or orthotics can provide support and stability to joints, reducing the risk of dislocations and injuries. In some cases, surgical interventions may be necessary to address severe joint instability or correct deformities.
- Skin care: Gentle skin care practices, including keeping the skin moisturized, avoiding excessive sun exposure, and protecting the skin from trauma or injury, can help manage skin-related symptoms such as fragility, easy bruising, or scarring.
- Gastrointestinal management: Dietary modifications, including a high-fiber diet and adequate hydration, can help manage gastrointestinal symptoms like constipation. In some cases, medications or interventions may be recommended by a gastroenterologist to address specific gastrointestinal issues.
- Cardiovascular monitoring and management: Regular monitoring of the cardiovascular system is essential, especially in individuals with vascular EDS. Collaboration with a cardiologist is important to assess cardiac function, monitor blood pressure, and manage any cardiovascular complications that may arise.
- Psychological support: EDS can have a significant impact on mental health, and individuals may benefit from supportive counseling, cognitive-behavioral therapy, or support groups to manage the emotional and psychological aspects of living with a chronic condition.
- Genetic counseling and family planning: Genetic counseling can provide individuals and their families with information about the inheritance pattern, reproductive options, and guidance for family planning.
Lifestyle modifications, including proper body mechanics, avoidance of high-risk activities, and maintaining a healthy weight, can help minimize the risk of injuries and improve overall well-being.




Well-written and easy to understand.
Your expertise really shines through in this article. The practical tips and insights you’ve shared are going to be very useful for my work.
I’m always learning something new from your blog.
This is such a valuable resource. I’ve learned so much from this post, and I appreciate the practical advice you’ve shared.
Your expertise really shines through in this article. The practical tips and insights you’ve shared are going to be very useful for my work.
Thank you for your articles. They are very helpful to me. May I ask you a question?
Thank you for writing this article. I appreciate the subject too.