INTRODUCTION:
Dyslipidemia refers to an abnormal level of lipids (fats) in the blood. It is a broad term that encompasses various lipid abnormalities, including high levels of total cholesterol, low-density lipoprotein cholesterol (LDL-C), triglycerides, or low levels of high-density lipoprotein cholesterol (HDL-C). Dyslipidemia is a significant risk factor for the development of atherosclerosis, heart disease, and other cardiovascular conditions. Here’s an overview of dyslipidemia:
TYPES OF DISLIPIDEMIA:
- Hypercholesterolemia: Characterized by high levels of total cholesterol and/or LDL-C. LDL-C is commonly referred to as “bad” cholesterol as it contributes to plaque buildup in the arteries.
- Hypertriglyceridemia: Involves elevated levels of triglycerides, which are a type of fat in the blood. High triglyceride levels are associated with increased cardiovascular risk, especially when combined with low levels of HDL-C.
- Low HDL Cholesterol: Low levels of HDL-C, often referred to as “good” cholesterol, can also contribute to dyslipidemia. HDL-C helps remove excess cholesterol from the blood, protecting against atherosclerosis.
CAUSES AND RISK FACTORS:
- Unhealthy Diet: Consuming a diet high in saturated fats, trans fats, and cholesterol can contribute to dyslipidemia.
- Sedentary Lifestyle: Lack of physical activity can lower HDL-C levels and lead to dyslipidemia.
- Obesity: Excess weight, particularly around the waist, is associated with dyslipidemia.
- Genetics: Some individuals may have genetic disorders that predispose them to dyslipidemia.
- Diabetes: People with diabetes often have dyslipidemia, characterized by high triglyceride levels and low HDL-C levels.
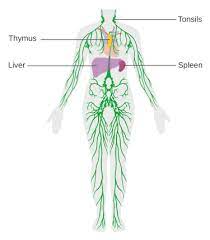
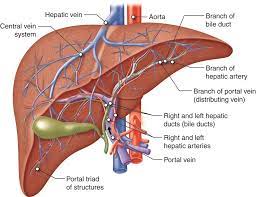
- Certain Medical Conditions: Hypothyroidism, kidney disease, liver disease, and certain hormonal disorders can contribute to dyslipidemia.
DIAGNOSING TESTS INCLUDE:
To diagnose dyslipidemia, various blood tests are conducted to assess the lipid profile and determine the levels of different types of cholesterol and triglycerides. The following tests are commonly used:
- a. Total Cholesterol: This measures the overall amount of cholesterol in the blood, including LDL (bad) cholesterol, HDL (good) cholesterol, and a fraction of triglycerides.b. LDL Cholesterol: LDL cholesterol is considered “bad” cholesterol as it contributes to the formation of plaque in the arteries.c. HDL Cholesterol: HDL cholesterol is considered “good” cholesterol as it helps remove LDL cholesterol from the bloodstream and reduces the risk of heart disease.d. Triglycerides: Triglycerides are a type of fat found in the blood. Elevated triglyceride levels are associated with increased cardiovascular risk.
TRIGLYCERIDES- BELOW 150mg/dil
HDL – above 50mg/dil
LDL – below 100 mg/dil and in some cases like diabtes mellitus and vascular complications less than 70 mg/dil is advised.
VLDL- 2-30 mg/dl
- Non-HDL Cholesterol: Non-HDL cholesterol is calculated by subtracting HDL cholesterol from the total cholesterol. It provides information about the levels of cholesterol-containing particles, including LDL cholesterol.
- Apolipoprotein B (apoB): ApoB is a protein that is present in LDL cholesterol and other atherogenic lipoproteins. Measuring apoB levels can provide a more accurate assessment of cardiovascular risk compared to LDL cholesterol alone.
- High Sensitivity C-Reactive Protein (hsCRP): hsCRP is a marker of inflammation in the body. Elevated hsCRP levels may indicate an increased risk of heart disease, particularly in combination with dyslipidemia.
- Lp(a) Lipoprotein: Lp(a) lipoprotein is a specific type of LDL cholesterol that is genetically determined. Elevated levels of Lp(a) can increase the risk of cardiovascular disease.
These tests are typically performed after fasting for 9-12 hours to obtain accurate measurements. It’s important to note that specific testing protocols may vary based on individual circumstances and the recommendations of healthcare professionals. Based on the test results, healthcare providers can assess the presence and severity of dyslipidemia and develop an appropriate treatment plan.
TREATMENT AND MANAGEMENT:
The treatment and management of dyslipidemia aim to reduce the risk of cardiovascular events and maintain healthy lipid levels. Common approaches include:
- Lifestyle Modifications: Adopting a heart-healthy diet, increasing physical activity, losing weight (if overweight or obese), and quitting smoking can help improve lipid profiles.
- Medications: In cases where lifestyle modifications alone are insufficient, healthcare professionals may prescribe lipid-lowering medications, such as statins, fibrates, niacin, or cholesterol absorption inhibitors. The choice of medication depends on individual risk factors, lipid levels, and overall health.
- Regular Monitoring: Regular lipid panel tests are necessary to assess lipid levels and gauge the effectiveness of lifestyle changes and medications.
- Managing Underlying Conditions: Addressing and managing underlying conditions such as diabetes, hypertension, and hypothyroidism can help improve dyslipidemia.
- Risk Factor Management: Controlling other cardiovascular risk factors like high blood pressure, diabetes, and smoking is crucial in managing dyslipidemia.
It’s essential to work closely with healthcare professionals to determine the appropriate treatment plan for dyslipidemia based on individual circumstances and medical history. Regular monitoring and follow-up visits are important to track progress and make necessary adjustments to the management approach.