INTRODUCTION:
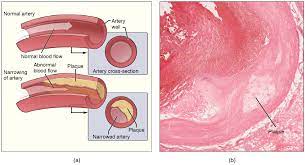
Atherosclerosis is a condition characterized by the buildup of plaque inside the arteries. It is a type of arteriosclerosis, which refers to the hardening and narrowing of arteries. Atherosclerosis typically develops over many years and is a leading cause of heart disease, stroke, and other cardiovascular problems. Here’s an overview of atherosclerosis
CAUSES:
The exact cause of atherosclerosis is not fully understood, but it is believed to involve several factors, including:
- High Cholesterol: Elevated levels of LDL (bad) cholesterol in the blood can contribute to the formation of plaque.
- Inflammation: Chronic inflammation within the blood vessels can promote the accumulation of plaque.
- High Blood Pressure: Hypertension can damage the inner lining of the arteries, making them more susceptible to plaque buildup.
- Smoking: Tobacco smoke damages blood vessels and accelerates the development of atherosclerosis.
- Diabetes: People with diabetes are at a higher risk of developing atherosclerosis due to increased blood sugar levels and other metabolic changes.
- Genetics: Family history and genetic factors can predispose individuals to atherosclerosis.
PROGRESSION :
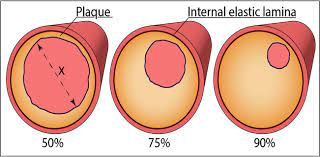
Atherosclerosis progresses through several stages:
- Endothelial Injury: Damage to the inner lining of the arteries triggers an inflammatory response.
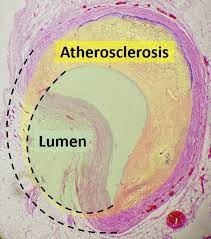
- Plaque Formation: LDL cholesterol particles penetrate the damaged arterial walls and accumulate, leading to the formation of fatty deposits called plaques.
- Plaque Growth: The plaques continue to accumulate cholesterol, calcium, and other substances, growing in size and narrowing the arterial lumen.
- Plaque Rupture: A vulnerable plaque can rupture, exposing its contents to the bloodstream. This triggers the formation of blood clots, which can partially or completely block the blood flow.
CONSEQUENCES AND COMPLICATIONS:
Atherosclerosis can lead to various complications, including:
- Coronary Artery Disease: When atherosclerosis affects the coronary arteries supplying the heart, it can cause angina (chest pain) or lead to a heart attack.
- Carotid Artery Disease: Atherosclerosis in the carotid arteries that supply blood to the brain can increase the risk of stroke.
- Peripheral Artery Disease: Narrowed arteries in the limbs can result in poor blood circulation, leading to pain, ulcers, and difficulty healing wounds.
- Aneurysms: Weakened arterial walls can bulge and form aneurysms, which can rupture and cause life-threatening bleeding.
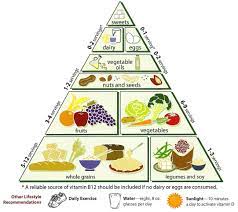
FOODS TAKEN IN ATHEROSCLEROTIC CONDITION:
When managing atherosclerosis, it’s important to adopt a heart-healthy diet that helps improve lipid profiles, reduces inflammation, and supports overall cardiovascular health. Here are some foods to include in your diet:
- Fatty Fish: Salmon, mackerel, trout, and sardines are rich in omega-3 fatty acids, which have anti-inflammatory properties and can help lower triglyceride levels.
- Fiber-Rich Foods: Include plenty of fruits, vegetables, whole grains, and legumes in your diet. These foods are high in soluble fiber, which can help lower LDL cholesterol levels. Examples include apples, oranges, berries, broccoli, spinach, oats, brown rice, and beans.
- Healthy Fats: Incorporate foods that contain monounsaturated fats and polyunsaturated fats, such as olive oil, avocados, nuts (almonds, walnuts), and seeds (flaxseeds, chia seeds). These fats can help improve cholesterol levels.
- Plant Sterols and Stanols: Foods fortified with plant sterols and stanols, such as some margarines, may help lower LDL cholesterol levels.
- Green Tea: Green tea contains antioxidants that can help reduce inflammation and improve blood lipid profiles.
- Garlic: Garlic has been shown to have cholesterol-lowering and anti-inflammatory effects. Include fresh garlic in your cooking or consider garlic supplements (under medical supervision).
- Berries: Blueberries, strawberries, raspberries, and other berries are rich in antioxidants and can help reduce inflammation.
- Dark Chocolate: Dark chocolate (at least 70% cocoa) in moderation may have heart-healthy benefits due to its antioxidants. However, be mindful of portion sizes and opt for dark chocolate with minimal added sugars.
- Tomatoes: Tomatoes are rich in lycopene, an antioxidant that may help reduce the risk of atherosclerosis. Cooked tomatoes or tomato products like tomato sauce and tomato paste are particularly beneficial.
- Nuts: Almonds, walnuts, pistachios, and other nuts are high in healthy fats, fiber, and plant sterols. They can help improve cholesterol levels when consumed in moderation.
It’s important to note that while these foods can be beneficial in managing atherosclerosis, they should be part of an overall balanced diet. Additionally, individual dietary recommendations may vary based on specific health conditions and medications, so it’s always best to consult with a healthcare professional or a registered dietitian for personalized dietary advice.
TESTS TO EVALUATE ATHEROMA:
To assess the severity of atherosclerosis and the presence of atheroma (plaque) in blood vessels, various tests and imaging techniques can be used. Here are some common diagnostic tests:
- Angiography: This invasive procedure involves injecting a contrast dye into the blood vessels and taking X-ray images. It can help visualize the narrowing or blockage caused by atherosclerotic plaques.
- Computed Tomography Angiography (CTA): CTA uses a combination of X-rays and computer technology to create detailed images of the blood vessels. It can provide information about the extent and severity of atherosclerosis.
- Magnetic Resonance Angiography (MRA): MRA uses magnetic fields and radio waves to produce images of blood vessels. It can help identify areas of narrowing or blockage caused by atherosclerotic plaques.
- Intravascular Ultrasound (IVUS): IVUS involves inserting a catheter with an ultrasound probe into the blood vessel. It provides detailed images of the vessel walls, allowing for the measurement of plaque size, composition, and severity.
- Coronary Calcium Scoring: This non-invasive test uses a specialized computed tomography (CT) scan to measure the amount of calcified plaque in the coronary arteries. It provides a calcium score, which is an indicator of the overall burden of atherosclerosis.
- Carotid Intima-Media Thickness (CIMT): CIMT is an ultrasound-based test that measures the thickness of the inner layers of the carotid arteries. Increased thickness can indicate the presence of atherosclerosis.
- Ankle-Brachial Index (ABI): ABI measures the blood pressure in the arms and ankles to assess peripheral artery disease. A lower index can indicate atherosclerotic narrowing in the lower extremities.
- Blood Tests: Certain blood tests can provide information about the presence and severity of atherosclerosis. These include high-sensitivity C-reactive protein (hsCRP) to measure inflammation, lipoprotein(a) [Lp(a)] to assess genetic risk, and other markers of lipid profile and inflammation.
These tests and imaging techniques can help healthcare professionals evaluate the severity of atherosclerosis and plan appropriate treatment strategies. The choice of test may depend on factors such as symptoms, risk factors, and the specific blood vessels being assessed. Your healthcare provider will determine the most appropriate tests based on your individual circumstances.
PREVENTION AND TREATMENT:
Preventing or managing atherosclerosis involves:
- Adopting a Healthy Lifestyle: This includes maintaining a balanced diet, regular physical activity, maintaining a healthy weight, avoiding smoking, and managing conditions like high blood pressure, cholesterol, and diabetes.
- Medications: Depending on the individual’s risk factors and health status, healthcare professionals may prescribe medications such as statins to manage cholesterol, antiplatelet drugs to reduce clot formation, and blood pressure-lowering medications.
- Procedures: In severe cases, procedures like angioplasty with stenting or coronary artery bypass grafting (CABG) may be necessary to restore blood flow in the affected arteries.
It’s important to work closely with healthcare professionals to assess your risk factors, undergo regular check-ups, and receive appropriate treatment and lifestyle guidance to prevent or manage atherosclerosis.