What is Malaria?
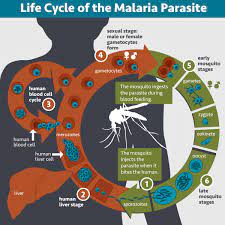
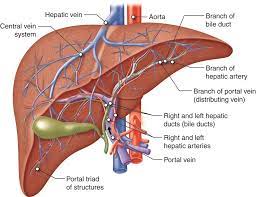
Malaria is a serious infectious disease caused by parasites that are transmitted to people through the bites of infected female Anopheles mosquitoes. Once an infected mosquito bites a person, the parasites multiply in the person’s liver before infecting and destroying red blood cells. This can cause fever, chills, flu-like symptoms, and in severe cases, organ failure and death.
The disease can be prevented by taking measures to avoid mosquito bites, such as using insect repellent and sleeping under mosquito nets. Treatment for malaria typically involves antimalarial medication, which can help to reduce the severity of symptoms and prevent complications.
SYMPTOMS OF MALARIA
The symptoms of malaria can vary depending on the species of Plasmodium parasite causing the infection and the individual’s immune response. The most common symptoms of malaria include:
- Fever: Fever is often the first and most prominent symptom of malaria. It may occur in cycles, with fever spikes followed by periods of normal or lower body temperature.
- Chills: Chills usually accompany the fever and may be severe, causing shaking and shivering.
- Headache: Malaria can cause intense headaches, which are often described as throbbing or pulsating.
- Muscle aches: Generalized body aches and muscle pain are common symptoms of malaria.
- Fatigue: Malaria can cause extreme tiredness and fatigue, even with mild physical activity.
- Sweating: Excessive sweating, especially during the fever episodes, is a characteristic symptom of malaria.
- Nausea and vomiting: Some individuals with malaria may experience nausea, vomiting, or a loss of appetite.
- Abdominal pain: Malaria can cause abdominal discomfort or pain, which may be accompanied by diarrhea in some cases.
- Anemia: Malaria can lead to a decrease in red blood cells, resulting in anemia. Symptoms of anemia include weakness, dizziness, and shortness of breath.
- Jaundice: In severe cases of malaria, a yellow discoloration of the skin and eyes (jaundice) may occur due to liver dysfunction.
It’s important to note that the symptoms of malaria can be similar to other illnesses, so a proper diagnosis is crucial. If you suspect you have malaria or have been in a malaria-endemic area and are experiencing these symptoms, it’s essential to seek medical attention for diagnosis and appropriate treatment.
Although malaria is treatable if caught early, it remains a major public health threat, mostly children under the age of five.
TRANSMISSION OF MALARIA:
Malaria is a potentially life-threatening infectious disease caused by parasites of the Plasmodium genus. It is transmitted to humans through the bites of infected female Anopheles mosquitoes.
The symptoms of malaria typically include fever, headache, chills, muscle aches, and fatigue. If left untreated, it can progress to severe illness, leading to complications such as organ failure, anemia, and even death.
There are several species of Plasmodium parasites that can cause malaria, with Plasmodium falciparum being the most deadly. Other species include Plasmodium vivax, Plasmodium malaria, and Plasmodium ovale. Each species has its own distinct characteristics and geographic distribution.
DIAGNOSTIC FACTORS
Blood tests are crucial for diagnosing malaria. There are different types of blood tests used to detect and confirm the presence of malaria parasites in the body. The two main types of blood tests for malaria are:
- Rapid Diagnostic Tests (RDTs): RDTs are simple, rapid, and easy-to-use diagnostic tests that can detect malaria antigens in the blood. These tests provide quick results within 15 to 20 minutes. RDTs work by detecting specific proteins or antigens produced by the malaria parasites in a small blood sample taken from a finger prick. RDTs are particularly useful in areas with limited laboratory facilities.
- Microscopic Examination of Blood Smears: This is considered the gold standard for malaria diagnosis. A small blood sample is collected through a finger prick or venous puncture and stained with special dyes. The stained blood smear is then examined under a microscope by a trained technician or healthcare professional. They look for the presence of malaria parasites and identify the species of Plasmodium causing the infection. Microscopic examination allows for a more detailed analysis of the parasites and can determine the parasite density in the blood.
It’s important to note that timing is crucial for accurate diagnosis. Malaria parasites show periodicity in their life cycle, and the concentration of parasites in the bloodstream may vary at different times of the day. Thus, multiple blood samples may be required for accurate diagnosis, especially if initial tests are negative but clinical suspicion remains high.
If you suspect you have malaria or have been exposed to malaria-endemic areas and are experiencing symptoms, it’s important to seek medical attention. A healthcare professional will be able to perform the necessary blood tests and provide an accurate diagnosis for appropriate treatment.
FOODS TO BE TAKEN :
During malaria, it’s important to maintain a balanced diet that provides essential nutrients to support your immune system and aid in recovery. Here are some general dietary recommendations:
- Adequate hydration: Drink plenty of fluids, such as water, herbal teas, and clear soups, to stay hydrated and prevent dehydration, especially if you have a fever and are experiencing sweating.
- Nutrient-rich foods: Consume a variety of nutrient-rich foods to support your immune system and overall health. Include fruits, vegetables, whole grains, lean proteins, and healthy fats in your meals.
- Iron-rich foods: Malaria can cause anemia, so it’s important to include iron-rich foods in your diet. Good sources of iron include red meat, poultry, fish, legumes, dark leafy greens, and fortified cereals.
- Vitamin C: Foods rich in vitamin C can help boost your immune system and enhance iron absorption. Include citrus fruits (such as oranges, grapefruits, and lemons), berries, kiwi, tomatoes, bell peppers, and leafy greens in your diet.
- Protein-rich foods: Protein is important for tissue repair and recovery. Include lean meats, poultry, fish, eggs, dairy products, legumes, nuts, and seeds in your meals.
- Antioxidant-rich foods: Antioxidants can help reduce inflammation and support the immune system. Include foods like berries, cherries, dark chocolate, spinach, kale, and colorful fruits and vegetables.
- Healthy fats: Include sources of healthy fats, such as avocados, nuts, seeds, and olive oil, in your diet to support overall health and provide energy.
- Avoid excessive sugar and processed foods: Limit your intake of sugary foods, processed snacks, and beverages as they can weaken the immune system and hinder the recovery process.
It’s important to note that these dietary recommendations are general in nature. If you have specific dietary restrictions, allergies, or underlying health conditions, it’s best to consult with a healthcare professional or a registered dietitian for personalized dietary advice.
PREVENTION
Prevention of malaria primarily involves mosquito control measures such as the use of insecticide-treated bed nets, indoor residual spraying, and environmental management to reduce mosquito breeding sites. Additionally, chemoprophylaxis (taking antimalarial drugs) is often recommended for travelers to malaria-endemic regions.
TREATMENT
The treatment of malaria typically involves the use of antimalarial medications, which vary depending on the species of Plasmodium causing the infection and the severity of the disease. Artemisinin-based combination therapies (ACTs) are commonly used as the first-line treatment for uncomplicated malaria caused by Plasmodium falciparum.
WHEN TO BE AFRAID OF MALARIA
Malaria is a serious and potentially life-threatening disease, particularly if left untreated or if complications arise. It’s important to be aware of certain situations or conditions that may increase the risk and severity of malaria. Here are some scenarios when you should be cautious and take malaria seriously:
- Traveling to endemic areas: If you are planning to travel to regions where malaria is prevalent, especially in tropical and subtropical regions, it’s important to be aware of the risk and take appropriate preventive measures. Consult with a healthcare professional or a travel medicine specialist well in advance to obtain information about malaria prevention, including antimalarial medications and mosquito bite prevention strategies.
- Living in endemic areas: If you reside in an area where malaria is endemic, it’s crucial to take consistent measures to protect yourself from mosquito bites, such as using bed nets, wearing protective clothing, and utilizing insect repellents.
- Lack of immunity: People who are not exposed to malaria regularly or have not built up immunity are at higher risk of developing severe malaria. This includes travelers from non-endemic areas and individuals relocating to malaria-endemic regions.
- Certain population groups: Certain population groups may be more vulnerable to severe malaria, including young children, pregnant women, elderly individuals, and those with weakened immune systems, such as people living with HIV/AIDS.
- Delayed diagnosis and treatment: Delaying the diagnosis and treatment of malaria can lead to more severe symptoms and complications. If you experience symptoms such as fever, chills, headache, and muscle aches, particularly after being in a malaria-endemic area, it is important to seek medical attention promptly for proper diagnosis and treatment.
- Drug-resistant malaria: In some regions, certain strains of malaria parasites have developed resistance to commonly used antimalarial medications. It’s important to be aware of drug resistance patterns in the area you are in or traveling to and ensure that the prescribed antimalarial medications are effective against the local strains.
If you have concerns about malaria or believe you may have been exposed to the disease, it is always best to seek medical advice from a healthcare professional. They can provide accurate diagnosis, appropriate treatment, and guidance based on your specific situation and medical history.