Introduction
It is one of the leading causes of death globally, and despite advancements in medical research, the number of cases continues to rise each year. The importance of discussing this topic in an engaging and informative way cannot be emphasized enough, as it can help raise awareness and promote early detection.
What is lung cancer?
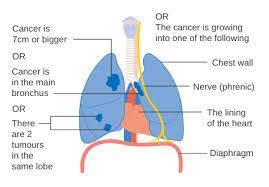
Lung cancer is a type of cancer that begins in the lungs. It occurs when abnormal cells grow out of control and form a tumor. These tumors can interfere with the normal function of the lungs, making it difficult to breathe.
There are two main types of lung cancer: non-small cell lung cancer and small cell lung cancer. Non-small cell lung cancer is the most common type, accounting for about 85% of all cases.
Lung cancer develops when cells in the lungs mutate or change in some way. This mutation causes the cells to grow and divide at an accelerated rate, forming a mass or tumor. The exact cause of these mutations is not always known, but smoking is the leading cause of lung cancer. Other risk factors include exposure to secondhand smoke, air pollution, and radon gas. In some cases, lung cancer may be caused by genetic factors.
Symptoms
Lung cancer can be difficult to detect in its early stages, as many of the symptoms are similar to those of other respiratory illnesses. However, some common symptoms of lung cancer include persistent coughing, shortness of breath, chest pain, hoarseness, and unexplained weight loss.
It is important to seek medical attention if any of these symptoms are present, as early detection is key to successful treatment.
Ignoring these symptoms can lead to the cancer spreading to other parts of the body, making it more difficult to treat.
Real-life examples of the impact of these symptoms on patients and their families can help illustrate the importance of seeking medical attention.
Risk Factors
Lung cancer is a complex disease caused by a combination of genetic and environmental factors. Some of the most common risk factors for lung cancer include smoking, exposure to secondhand smoke, air pollution, and radon gas. Smoking is the leading cause of lung cancer, accounting for approximately 85% of all cases. Other lifestyle factors that can increase the risk of developing lung cancer include heavy alcohol consumption and a diet high in saturated fats.
In addition to lifestyle factors, there are also genetic factors that can increase the risk of developing lung cancer. Certain genetic mutations, such as those found in the EGFR gene, have been linked to an increased risk of lung cancer. Family history of lung cancer can also be a risk factor, as some people may inherit certain genetic mutations that increase their susceptibility to the disease.
Diagnosis:
The diagnosis of lung cancer typically involves a combination of medical history evaluation, physical examination, imaging tests (such as X-rays, CT scans, or MRI scans), and a biopsy to examine a sample of lung tissue for cancerous cells. Once diagnosed, the cancer is staged to determine its extent and guide treatment decisions.
Diagnosing lung cancer typically involves a series of tests and procedures to evaluate the presence of cancer, determine the type and stage of the disease, and guide treatment decisions. Here are some commonly used diagnostic tests for evaluating lung cancer:
While blood tests alone cannot definitively diagnose lung cancer, they can provide valuable information to support the diagnostic process and help monitor the disease. Here are some blood tests that may be recommended for individuals suspected of having lung cancer:
BLOOD TESTS
Complete Blood Count Clearing the Air: Understanding and Fighting Lung Cancert (CBC):A CBC measures various components of the blood, including red blood cells, white blood cells, and platelets.
While it doesn’t directly detect lung cancer, it can help evaluate overall health and identify any abnormalities, such as anemia or infection, which may be associated with lung cancer or its complications.
- Tumor Marker Tests: Certain substances known as tumor markers may be elevated in the blood of individuals with lung cancer. These markers are not specific to lung cancer and can be elevated in other conditions as well. However, they can provide supportive information when combined with other diagnostic tests. The commonly used tumor markers for lung cancer include:
- Carcinoembryonic Antigen (CEA): Elevated levels of CEA can indicate the presence of lung cancer, although it can also be elevated in other cancers or non-cancerous conditions.
- Neuron-Specific Enolase (NSE): Increased levels of NSE may be associated with small cell lung cancer (SCLC) and can be used to monitor response to treatment.
- Progastrin-releasing peptClearing the Air: Understanding and Fighting Lung Canceride (ProGRP): Elevated ProGRP levels are more specific to small cell lung cancer (SCLC) and can be used in combination with other tests for diagnosis and monitoring.
- CYFRA 21-1: This marker is more commonly used in non-small cell lung cancer (NSCLC) and can help assess the response to treatment.
It’s important to note that tumor marker tests are not definitive diagnostic tools for lung cancer and should be used in conjunction with other diagnostic methods.
- Genetic Testing: In some cases, genetic testing may be recommended to detect specific genetic mutations or alterations that can guide treatment decisions. This can involve analyzing the DNA from a blood sample for mutations in genes such as EGFR, ALK, ROS1, BRAF, and others. These mutations can help determine if targeted therapies or immunotherapies may be appropriate.
- Liver and Kidney Function Tests: Liver function tests (LFTs) and kidney function tests (KFTs) may be conducted to evaluate the overall functioning of these organs. These tests help determine if lung cancer has spread to other parts of the body or if certain treatment options may be suitable based on organ function.
It’s important to remember that blood tests are just one aspect of the diagnostic process for lung cancer. They are typically used in conjunction with imaging tests, biopsies, and other diagnostic procedures to establish an accurate diagnosis and determine the best course of treatment. Consulting with a healthcare professional is essential to understand which tests are appropriate for an individual’s specific situation.
- Medical History and Physical Examination: A healthcare professional will begin by taking a detailed medical history, including information about symptoms, smoking history, exposure to risk factors, and family history of cancer. They will also perform a physical examination to assess general health and any specific signs related to lung cancer.
- Imaging Tests: Various imaging techniques are used to visualize the lungs and detect abnormalities. These tests may include:
- Chest X-ray: A basic imaging test that provides a two-dimensional image of the lungs to identify any abnormal masses or nodules.
- Computed Tomography (CT) Scan: A more detailed imaging test that creates cross-sectional images of the chest. CT scans can detect smaller nodules, determine their size and location, and evaluate the involvement of nearby structures.
- Magnetic Resonance Imaging (MRI) Scan: In certain cases, an MRI may be recommended to obtain more detailed images of the chest, particularly if there is a suspicion of tumor invasion into nearby structures.
- Positron Emission Tomography (PET) Scan: This test involves injecting a small amount of radioactive material into the body, which is absorbed by rapidly dividing cells, including cancer cells. A PET scan combined with a CT scan (PET-CT) helps identify areas of increased metabolic activity, indicating the presence of cancerous cells.
- Biopsy: A biopsy is a definitive procedure to confirm the presence of lung cancer by examining a sample of tissue or fluid. There are different types of biopsies, including:
- Needle Biopsy: A needle is inserted through the skin and guided to the lung tumor to obtain a tissue sample. This can be done using various techniques, such as fine-needle aspiration (FNA) or core needle biopsy.
- Bronchoscopy: A thin, flexible tube with a light and camera (bronchoscope) is passed through the mouth or nose and into the airways to visualize the lungs. During the procedure, the doctor may collect tissue samples or perform a bronchoalveolar lavage (BAL) to collect fluid for analysis.
- Surgical Biopsy: In some cases, a surgical procedure may be required to obtain a tissue sample directly from the lung or lymph nodes. This can be done through minimally invasive techniques (video-assisted thoracoscopic surgery or VATS) or through an open thoracotomy.
- Molecular Testing: Molecular testing is performed on the tissue samples obtained from biopsies to identify specific genetic mutations or alterations that can guide treatment decisions. This may include testing for mutations in genes like EGFR, ALK, ROS1, BRAF, or others.
- Staging: Once the presence of lung cancer is confirmed, further tests are performed to determine the stage of the disease, which helps in planning appropriate treatment strategies. Staging may involve additional imaging tests, such as CT scans, PET-CT scans, bone scans, or brain imaging.
It’s important to note that the specific diagnostic tests and procedures recommended may vary depending on individual circumstances and the judgment of the healthcare provider. A multidisciplinary approach involving oncologists, radiologists, pathologists, and other specialists is often employed to ensure accurate diagnosis and personalized treatment plans for patients with lung cancer.
Treatment Options
Lung cancer is a serious disease that requires prompt and effective treatment. There are several treatment options available, depending on the stage and type of cancer, as well as the patient’s overall health.
The treatment plan for lung cancer depends on various factors, including the type and stage of cancer, overall health, and individual preferences. The main treatment options include:
- Surgery: Surgical intervention aims to remove the tumor and nearby affected tissues. It may involve removing a portion of the lung (lobectomy), the entire lung (pneumonectomy), or nearby lymph nodes.
- Radiation Therapy: This treatment utilizes high-energy radiation to target and destroy cancer cells. It can be used as the primary treatment or in combination with surgery or chemotherapy.
- Chemotherapy: Anti-cancer drugs are administered orally or intravenously to kill cancer cells. Chemotherapy is often used in advanced stages of lung cancer or when the cancer has spread to other parts of the body.
- Targeted Therapy: Targeted drugs are designed to specifically attack cancer cells while minimizing damage to healthy cells. They work by targeting specific mutations or genetic changes present in cancer cells.
- Immunotherapy: This treatment boosts the body’s immune system to recognize and attack cancer cells. It has shown promising results in certain cases of advanced lung cancer.
These treatments can have side effects, such as fatigue, nausea, and hair loss, but they are often necessary to ensure the best possible outcome for the patient.
Prevention and Early Detection
Preventing lung cancer starts with making healthy lifestyle choices. Quitting smoking is the most important step you can take to reduce your risk of developing lung cancer. Avoiding exposure to secondhand smoke, chemicals, and pollutants can also help lower your risk.
Early detection is key to successfully treating lung cancer. If you have a history of smoking or are experiencing any symptoms such as persistent coughing, shortness of breath, or chest pain, it is important to talk to your doctor. Regular screenings can also help detect lung cancer in its early stages.