WHAT IS DIABETES ?
Diabetes is a chronic disease characterized by high blood sugar levels that result from the body’s inability to produce or properly use insulin, a hormone that regulates blood sugar levels. According to the World Health Organization (WHO), approximately 422 million people worldwide have diabetes, and its prevalence is increasing rapidly, especially in low- and middle-income countries.
TYPES OF DIABETES:
There are two main types of diabetes: type 1 and type 2. Type 1 diabetes is an autoimmune disease in which the body’s immune system mistakenly attacks and destroys the insulin-producing cells in the pancreas. This type of diabetes usually develops in childhood or adolescence and requires lifelong insulin therapy. Type 2 diabetes, on the other hand, is the result of the body’s inability to properly use insulin, known as insulin resistance. This type of diabetes is strongly linked to lifestyle factors such as obesity, physical inactivity, and unhealthy diet, and can often be managed with lifestyle changes and medications.
CHANGES OCCUR INSIDE OUR BODY IN DIABETES
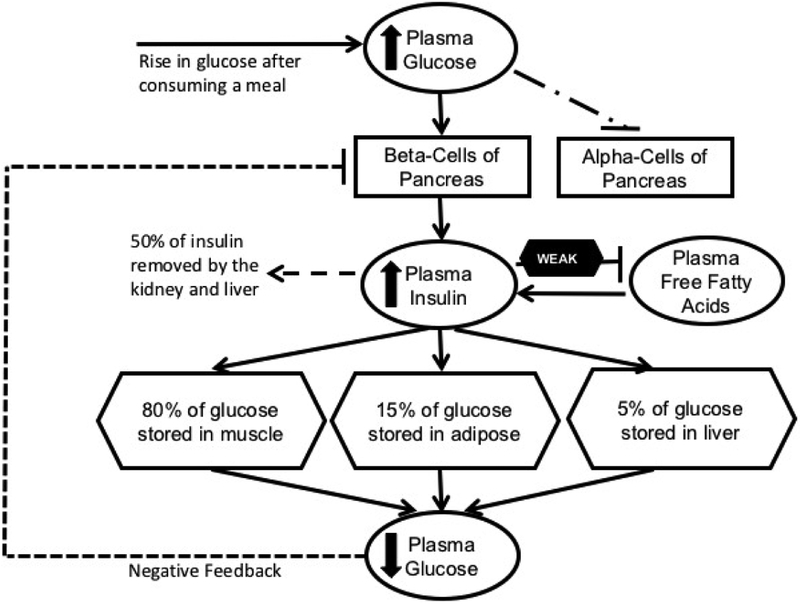
Diabetes is a metabolic disorder that occurs when the body is unable to produce enough insulin or effectively use the insulin it produces. Insulin is a hormone that regulates blood glucose levels, which is the primary source of energy for the body.
The two main types of diabetes are type 1 diabetes and type 2 diabetes. In type 1 diabetes, the body’s immune system attacks and destroys the cells in the pancreas that produce insulin, leading to a deficiency of insulin in the body. In type 2 diabetes, the body becomes resistant to the effects of insulin or produces insufficient amounts of insulin.
CHANGES THAT OCCUR INSIDE BODY IN TYPE 1 DIABETES MELLITUS
- Genetic Predisposition: Type 1 diabetes has a strong genetic component, although the exact genes involved are still being studied. Certain human leukocyte antigen (HLA) genotypes, specifically HLA-DR3 and HLA-DR4, are associated with an increased risk of developing type 1 diabetes. However, having these genes alone is not sufficient to cause the disease.
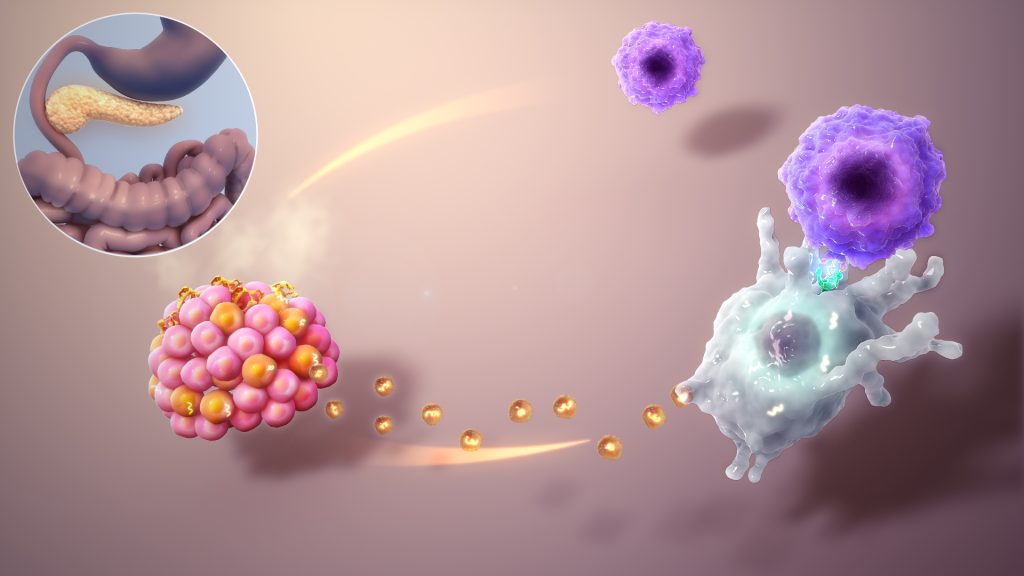
- Autoimmune Destruction of Beta Cells: The autoimmune theory suggests that an environmental trigger, such as a viral infection or dietary factor, initiates an autoimmune response in individuals with a genetic susceptibility. The immune system mistakenly identifies the insulin-producing beta cells in the pancreatic islets of Langerhans as foreign and launches an immune attack.
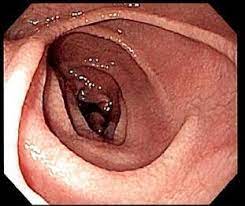
- Insulitis: Insulitis is the term used to describe the infiltration of immune cells, particularly T lymphocytes, into the pancreatic islets. These immune cells release cytokines and other mediators that induce inflammation and further attract more immune cells. The inflammatory process ultimately leads to the destruction of beta cells, resulting in a progressive decline in insulin production.
- Insulin Deficiency and Hyperglycemia: As the autoimmune destruction of beta cells continues, the insulin production becomes insufficient to maintain normal blood glucose control. This leads to elevated blood glucose levels (hyperglycemia) and the clinical manifestations of diabetes, such as increased thirst, frequent urination, weight loss, and fatigue.
- Islet Cell Antibodies: In most cases of type 1 diabetes, autoantibodies against beta cells and other pancreatic islet antigens can be detected in the blood. These autoantibodies, including anti-islet cell antibodies (ICA), anti-insulin antibodies (IAA), anti-glutamic acid decarboxylase antibodies (GAD), and others, serve as markers of autoimmune destruction and can be useful in the diagnosis and prediction of type 1 diabetes.
CHANGES THAT OCCUR INSIDE OUR BODY IN TYPE 2 DIABETES:
Regardless of the type of diabetes, the chronic hyperglycemia (high blood glucose) that results from the condition can lead to a wide range of complications affecting various organs and tissues in the body. These complications can include:
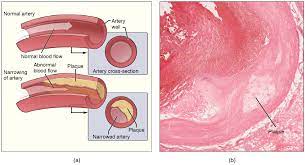
- Cardiovascular disease: Elevated blood glucose levels over an extended period can cause damage to the blood vessels, leading to the development of atherosclerosis (hardening of the arteries), which can increase the risk of heart attack and stroke.
- Neuropathy: Chronic hyperglycemia can cause damage to the nerves in the body, leading to numbness, tingling, and pain in the hands and feet.
- Nephropathy: High blood glucose levels can cause damage to the blood vessels in the kidneys, leading to kidney failure.
- Retinopathy: Elevated blood glucose levels can damage the blood vessels in the eyes, leading to vision impairment and even blindness.
- Diabetic ketoacidosis (DKA): This is a potentially life-threatening complication of type 1 diabetes that occurs when the body breaks down fat for energy in the absence of sufficient insulin, leading to the production of ketones that can cause the blood to become acidic.
REQUIRED LIFE STYLE CHANGES :
- DIET: People with diabetes need to eat a healthy and balanced diet that is low in sugar, saturated and trans fats, and refined carbohydrates. A diet rich in vegetables, fruits, whole grains, lean protein, and healthy fats can help manage blood sugar levels and reduce the risk of complications.
- Exercise: Regular physical activity is important for people with diabetes to control blood sugar levels, maintain a healthy weight, and improve overall health. Exercise can include activities such as walking, swimming, cycling, or strength training.
- Monitoring blood sugar levels: People with diabetes need to monitor their blood sugar levels regularly to ensure they are in a healthy range. This can involve self-monitoring with a blood glucose meter or continuous glucose monitoring (CGM) devices.
- Stress management: Stress can affect blood sugar levels in people with diabetes. Learning stress management techniques such as deep breathing, meditation, or yoga can help manage stress levels and improve overall well-being.
- Smoking cessation: Smoking can increase the risk of complications for people with diabetes. Quitting smoking can help reduce the risk of these complications and improve overall health.
NATURAL REMEDIES FOR DIABETES:
- Bitter gourd: Bitter gourd, also known as bitter melon, has been used for centuries to manage blood sugar levels. You can consume it as a juice, or include it in your meals by stir-frying or baking it.
- Cinnamon: Cinnamon has been shown to help regulate blood sugar levels. You can add cinnamon to your tea or coffee, sprinkle it on your oatmeal, or take a cinnamon supplement.
- Fenugreek: Fenugreek seeds are rich in fiber and have been shown to help lower blood sugar levels. You can soak the seeds in water overnight and drink the water in the morning.
- Amla: Amla, or Indian gooseberry, is a rich source of vitamin C and has been shown to improve insulin sensitivity. You can eat it raw, or drink its juice.
- Aloe vera: Aloe vera has anti-inflammatory and antioxidant properties, and has been shown to improve blood sugar levels in people with type 2 diabetes. You can drink aloe vera juice or add aloe vera gel to your smoothies.
- Gymnema sylvestra leaves are advised to chew early in the morning.
COMPLICATIONS OF DIABETES IF NOT TREATED:
Uncontrolled diabetes can lead to a range of complications that affect various organs and systems in the body. High blood sugar levels can damage the blood vessels, nerves, and organs over time, leading to cardiovascular disease, kidney disease, nerve damage, vision loss, and other health problems. In addition, people with diabetes are at increased risk of infections, particularly of the skin, urinary tract, and gums.
INFECTIONS IN DIABETES
Infections can have a significant impact on individuals with diabetes. Diabetes affects the body’s ability to regulate blood sugar levels, which can weaken the immune system and make people with diabetes more susceptible to infections. Here are some common infections associated with diabetes:
- Urinary tract infections (UTIs): UTIs are more common in people with diabetes, particularly in women. Elevated blood sugar levels create an environment that promotes bacterial growth in the urinary tract.
- Skin infections: People with diabetes are prone to skin infections, including bacterial and fungal infections. High blood sugar levels can impair the skin’s ability to function as a barrier against infections.
- Yeast infections: Yeast infections, such as vaginal yeast infections in women and oral thrush, are more common in individuals with diabetes. Elevated blood sugar levels provide a favorable environment for yeast to grow.
- Foot infections: Diabetes can cause peripheral neuropathy (nerve damage) and poor blood circulation, particularly in the feet. These conditions can lead to foot ulcers and infections, which can be challenging to treat and may result in serious complications.
- Respiratory infections: People with diabetes may be at a higher risk of respiratory infections, including pneumonia and influenza. Diabetes weakens the immune system, making individuals more vulnerable to these infections.
It’s important for individuals with diabetes to take steps to prevent infections. Good diabetes management, including maintaining healthy blood sugar levels, can help support a stronger immune system. Additionally, practicing good hygiene, such as regular handwashing, and receiving recommended vaccinations, such as the flu vaccine and pneumococcal vaccine, can help reduce the risk of infections.
If you have diabetes and suspect an infection, it’s crucial to seek medical attention promptly. Prompt treatment can help prevent the infection from worsening and potentially leading to complications. Your healthcare provider will be able to diagnose and recommend appropriate treatment options based on your specific situation.
DIABETES IN PREGNANCY:
Diabetes in pregnancy, also known as gestational diabetes mellitus (GDM), is a condition that affects pregnant women. It is characterized by high blood sugar levels that develop during pregnancy and typically resolves after childbirth. Here are some key points about diabetes in pregnancy:
- Prevalence: Gestational diabetes affects approximately 2-10% of pregnancies, depending on various factors such as the population studied and diagnostic criteria used.
- Causes: The exact cause of gestational diabetes is not known, but it is believed to be related to hormonal changes during pregnancy. The placenta produces hormones that can impair the action of insulin, resulting in insulin resistance.
- Risk factors: Several factors can increase the risk of developing gestational diabetes. These include being overweight or obese, having a family history of diabetes, previous history of gestational diabetes, being older than 25, certain ethnic backgrounds (e.g., Hispanic, African-American, Asian), and polycystic ovary syndrome (PCOS).
- Screening and diagnosis: Pregnant women are usually screened for gestational diabetes between 24 and 28 weeks of gestation. The most common screening test is the oral glucose tolerance test (OGTT), which involves drinking a glucose solution and having blood sugar levels measured at certain time intervals.
- Complications: If left uncontrolled, gestational diabetes can have several adverse effects on both the mother and the baby. It increases the risk of high blood pressure, preeclampsia (a potentially serious condition characterized by high blood pressure and damage to organs), and the need for a cesarean section. Babies born to mothers with gestational diabetes may be larger than average (macrosomia), which can increase the risk of birth injuries and complications during delivery. They may also have low blood sugar levels (hypoglycemia) shortly after birth.
- Management: Treatment for gestational diabetes involves lifestyle modifications, such as following a healthy diet, regular physical activity, and maintaining a healthy weight. Some women may require insulin or other medications to control their blood sugar levels. Regular monitoring of blood glucose levels is important to ensure they remain within a target range.
- Postpartum follow-up: After delivery, blood sugar levels usually return to normal. However, women who have had gestational diabetes are at an increased risk of developing type 2 diabetes later in life. It is recommended to undergo postpartum testing for diabetes and adopt a healthy lifestyle to reduce the risk.
If you suspect you have gestational diabetes or have any concerns about diabetes in pregnancy, it is essential to consult with your healthcare provider. They can provide a proper diagnosis and guidance on managing the condition to ensure the health and well-being of both you and your baby.
INSULIN THERAPY:
Insulin therapy is a treatment method used for managing diabetes, a chronic condition characterized by high blood sugar levels. Insulin is a hormone produced by the pancreas that helps regulate blood sugar. In people with diabetes, either the body does not produce enough insulin (Type 1 diabetes) or the body’s cells do not effectively respond to insulin (Type 2 diabetes).
Insulin therapy involves administering insulin to help control blood sugar levels and prevent complications associated with diabetes. It is typically prescribed for people with Type 1 diabetes and may also be used in some cases of Type 2 diabetes when other methods, such as oral medications or lifestyle changes, are not sufficient to control blood sugar levels.
Here are some key points about insulin therapy:
- Types of Insulin: There are several types of insulin available, including rapid-acting, short-acting, intermediate-acting, and long-acting insulin. The choice of insulin type depends on individual needs and the management plan recommended by the healthcare provider.
- Insulin Administration: Insulin can be administered using insulin pens, insulin pumps, or insulin syringes. The method of administration may vary based on personal preference, lifestyle, and the specific insulin regimen prescribed.
- Insulin Regimens: There are various insulin regimens that can be used, including multiple daily injections (MDI) and insulin pump therapy. MDI involves taking a combination of rapid-acting and long-acting insulin injections throughout the day. Insulin pumps deliver a continuous supply of insulin through a small device worn on the body.
- Blood Sugar Monitoring: Regular monitoring of blood sugar levels is essential when using insulin therapy. This helps determine the appropriate dosage of insulin and ensures blood sugar levels are within the target range.
- Carbohydrate Counting: Carbohydrate counting is often used in insulin therapy to match the insulin dosage with the amount of carbohydrates consumed. This technique helps maintain better control over blood sugar levels.
- Hypoglycemia: Insulin therapy carries a risk of hypoglycemia, or low blood sugar. It is important to be aware of the symptoms of hypoglycemia and have glucose tablets or another form of fast-acting sugar available to treat it if it occurs.
- Individualized Approach: Insulin therapy is highly individualized, and the specific insulin regimen and dosage will vary depending on factors such as age, lifestyle, overall health, and diabetes management goals. Regular communication with a healthcare provider is crucial to adjust the treatment plan as needed.
It’s important to note that the information provided here is a general overview, and the specifics of insulin therapy should be discussed with a healthcare professional who can provide personalized guidance based on an individual’s unique circumstances.
PREVENTIVE STEPS OF DIABETES:
Preventing diabetes involves healthy lifestyle choices such as regular physical activity, a healthy diet, and maintaining a healthy weight. For people with diabetes, managing blood sugar levels is critical in preventing complications. This involves monitoring blood sugar levels regularly, taking medications as prescribed, and making lifestyle changes to keep blood sugar levels within a healthy range.
MANAGEMENT OF DIABETES :
Diabetes management also includes regular check-ups with healthcare providers to monitor blood sugar levels, blood pressure, cholesterol levels, and other health markers. In addition, people with diabetes should receive regular eye exams, foot exams, and dental exams to detect and treat any complications early.
In conclusion, diabetes is a chronic disease that affects millions of people worldwide. It is a complex disease that requires ongoing management and monitoring to prevent complications. By making healthy lifestyle choices and working closely with healthcare providers, people with diabetes can lead healthy and fulfilling lives.